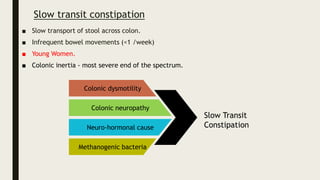
1) The document discusses the physiology and types of constipation including normal transit, slow transit, and dyssynergic defecation.
2) It provides guidelines for evaluating patients with constipation through history, physical exam, and tests to identify organic causes or characterize colonic transit time.
3) Key tests discussed are abdominal x-ray, colonic transit studies using radiopaque markers or wireless motility capsule, and anorectal manometry to identify dyssynergic defecation.