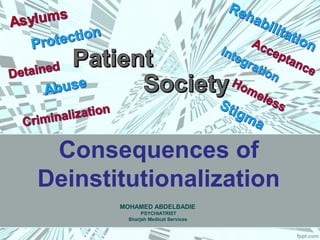
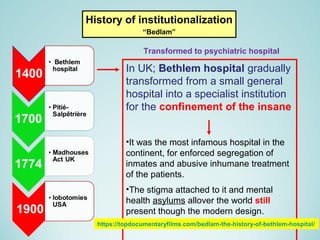
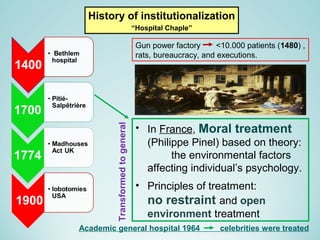
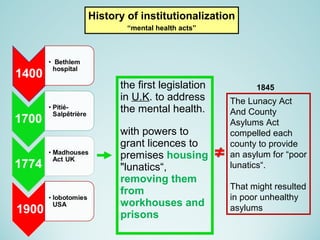
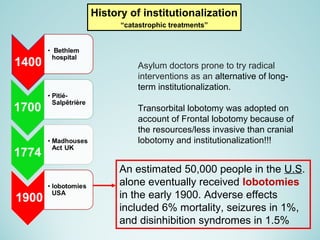
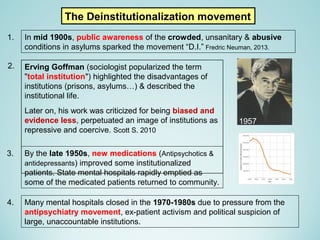
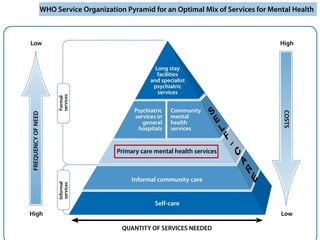
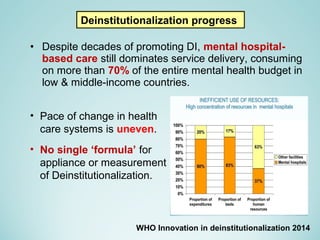
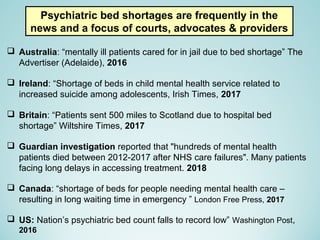
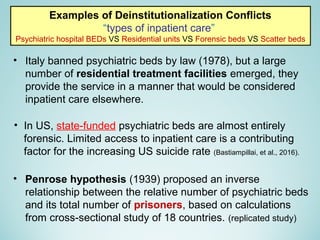
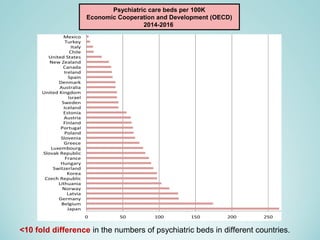
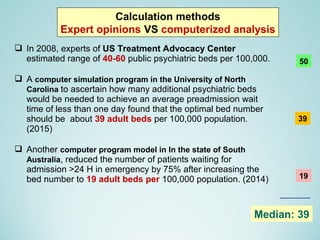
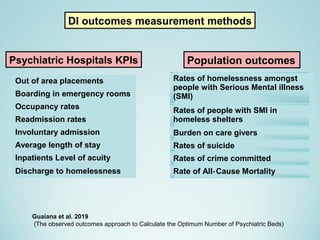
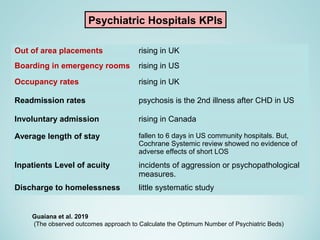
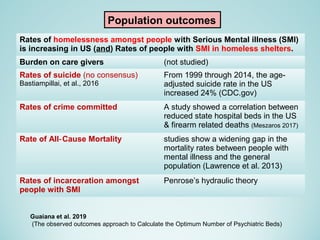
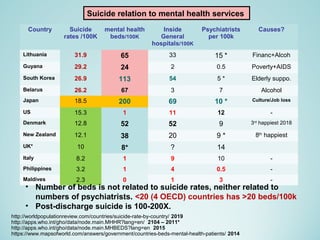
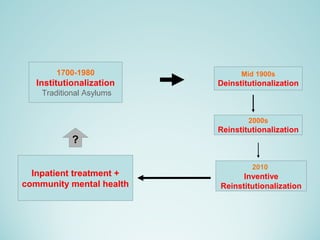
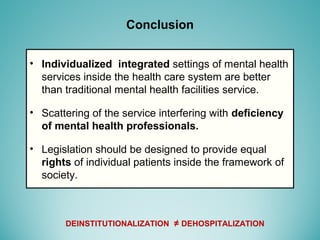
This document discusses the history of deinstitutionalization of mental health services. It describes how large psychiatric hospitals were gradually replaced by community-based services starting in the 1950s due to factors like new medications, poor conditions in hospitals, and civil rights movements. However, deinstitutionalization has faced challenges including shortages of beds and community services in many places. There is no consensus on optimal numbers of psychiatric beds, but most experts estimate around 39 beds per 100,000 people. Outcomes of deinstitutionalization like rates of homelessness, suicide, and crime are complex to assess with no clear relationship to number of beds or other services. The document concludes that an individualized, integrated approach within healthcare is better than traditional facilities