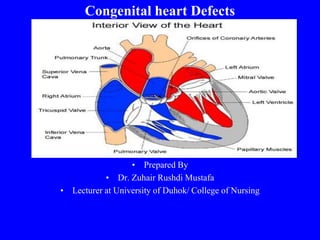
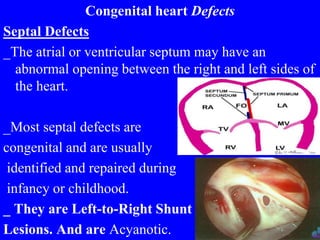
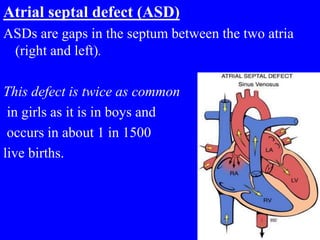
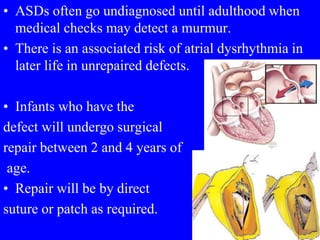
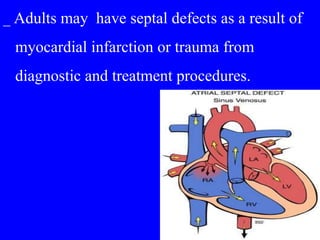
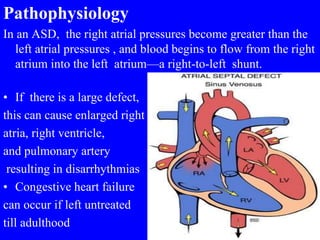
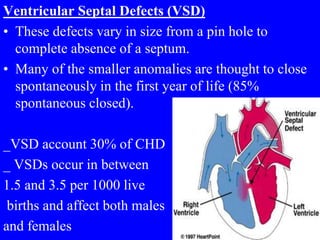
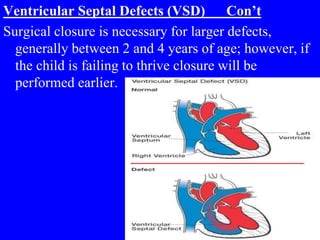
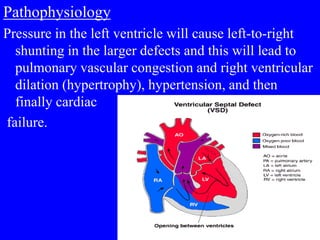
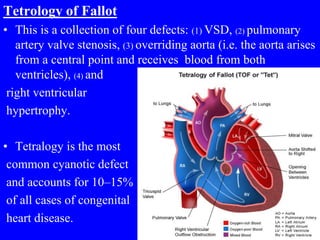
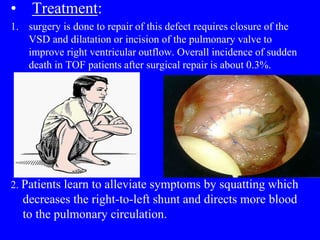
Congenital heart defects can be classified as acyanotic or cyanotic. Common acyanotic defects include ventricular septal defects and atrial septal defects. Common cyanotic defects include tetralogy of Fallot. Septal defects involve abnormal openings between the right and left sides of the heart. Atrial septal defects are more common in females and often go undiagnosed until adulthood. Ventricular septal defects vary in size and many small defects close spontaneously in the first year. Tetralogy of Fallot includes four defects and is the most common cyanotic defect. Surgical repair is often needed to correct congenital heart defects.