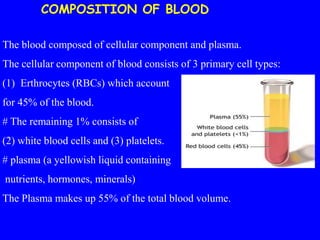
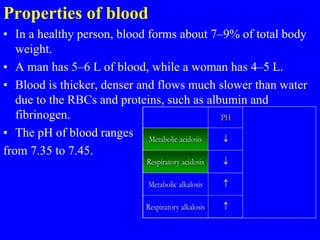
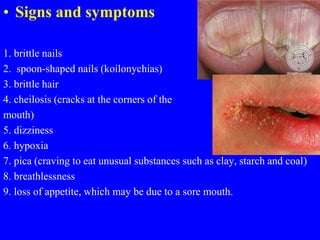
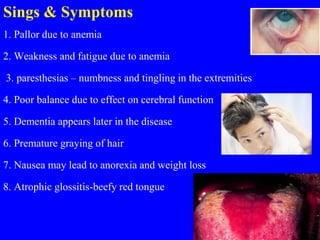
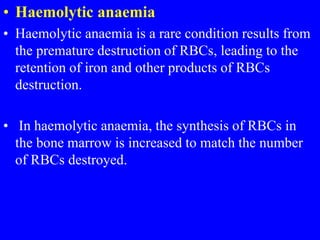
1. The document discusses various blood diseases including different types of anemia (microcytic, macrocytic, normocytic), their causes, signs and symptoms, and treatment approaches.
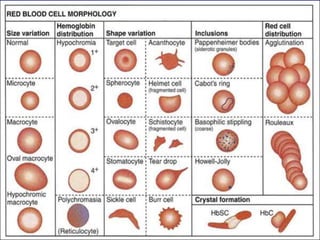
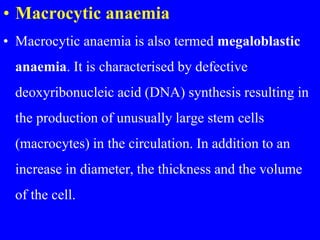
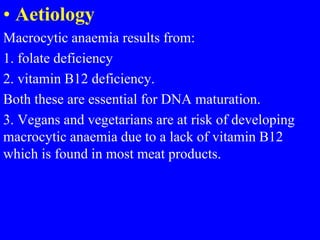
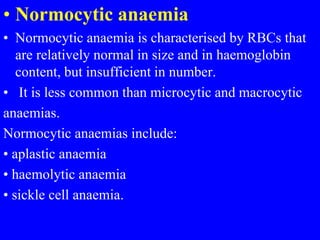
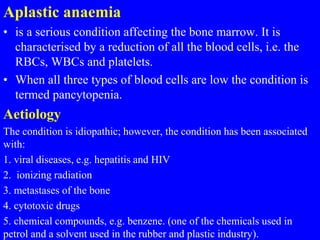
2. Microcytic anemias like iron deficiency anemia result in small red blood cells, while macrocytic anemias from folate or B12 deficiency produce large cells. Normocytic anemias maintain normal cell size.
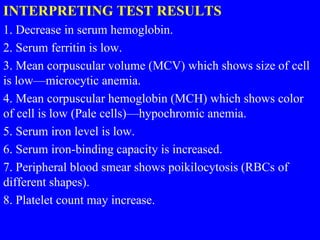
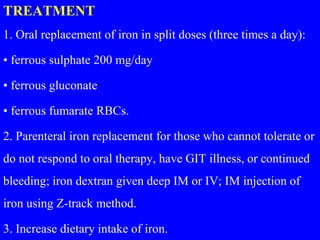
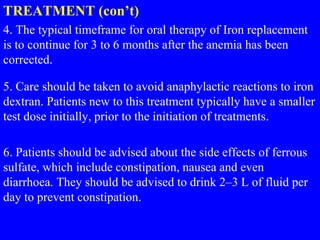
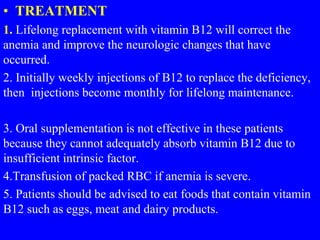
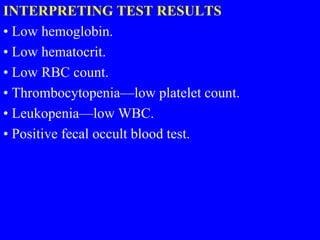
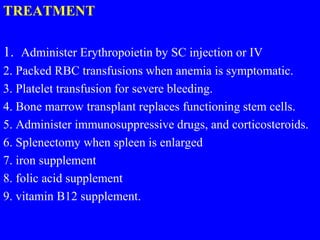
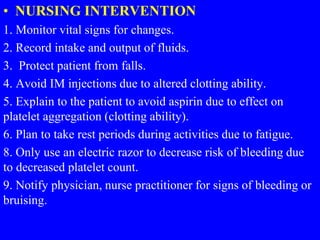
3. Diagnostic tests include complete blood counts and smears to identify cell types and sizes. Management involves treating the underlying cause, blood transfusions, and supplements.