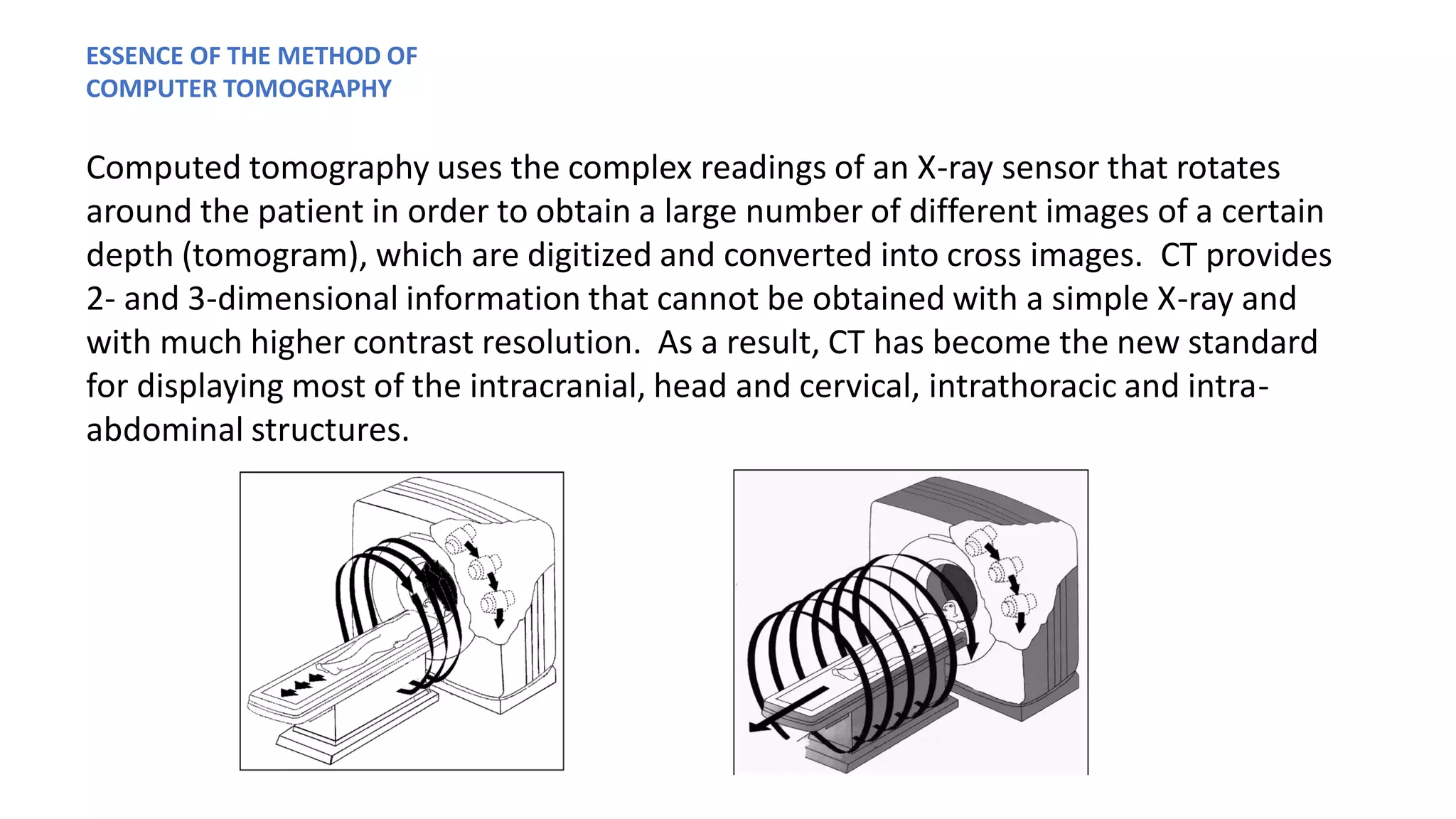
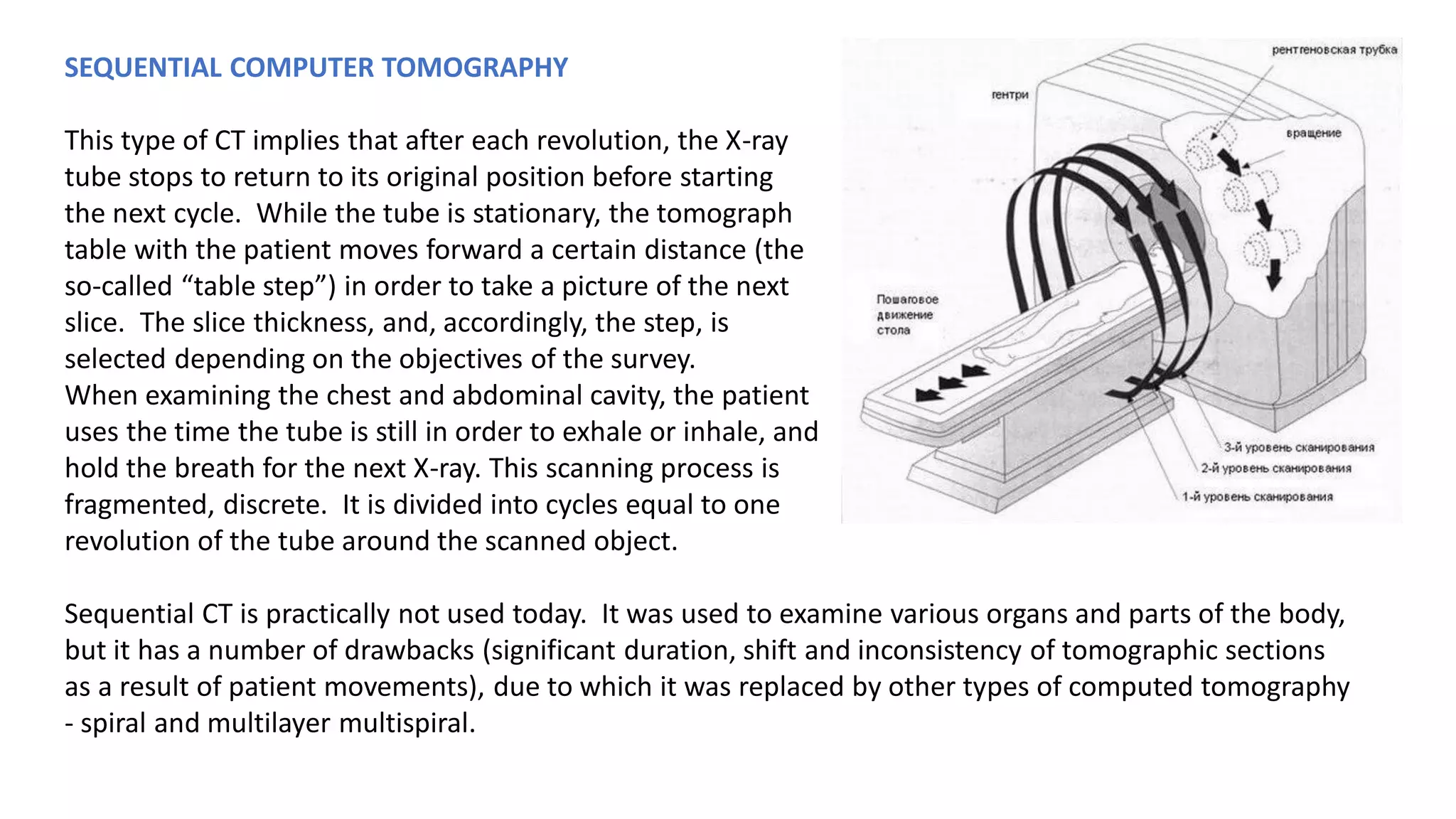
Computed tomography (CT) uses X-rays and computer processing to create cross-sectional images of the body. It was developed in the 1970s based on earlier work using X-rays and mathematical theories. CT provides detailed internal images without invasive surgery. It has become a standard medical imaging technique due to its high-resolution views of internal structures.