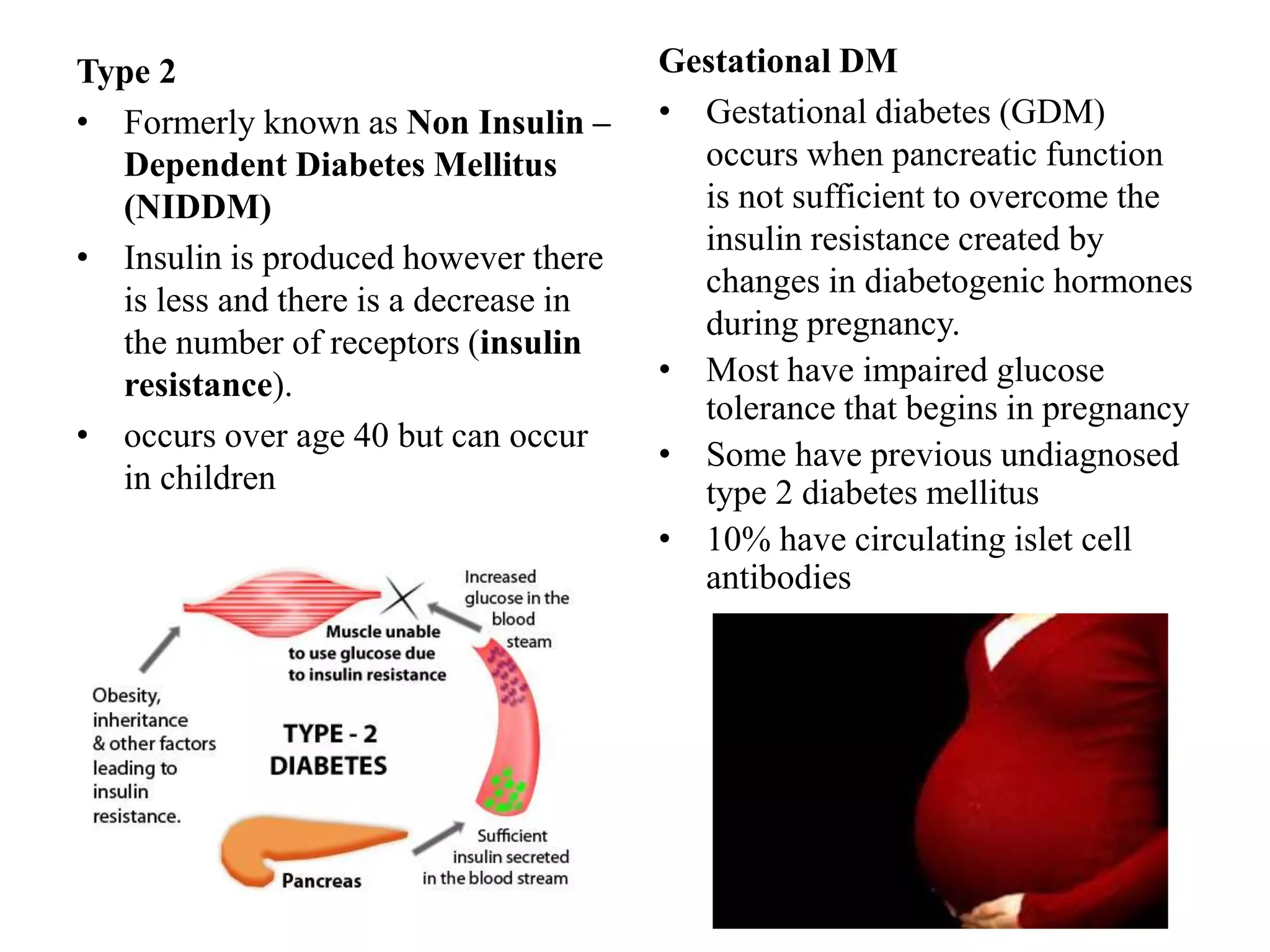
This document presents information on complications, management, and treatment of diabetes mellitus. It defines diabetes as a group of metabolic diseases involving high blood glucose levels due to inadequate insulin production or cells not responding to insulin. It discusses the types and classifications of diabetes, epidemiology, clinical manifestations, acute and chronic complications, and current pharmacological and non-pharmacological treatment approaches including insulin, oral hypoglycemic agents, lifestyle changes, and education. The goal of diabetes management is to eliminate hyperglycemia symptoms, reduce complications, and allow patients to live as normal a lifestyle as possible.