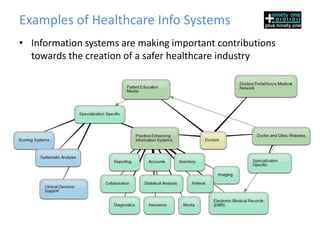
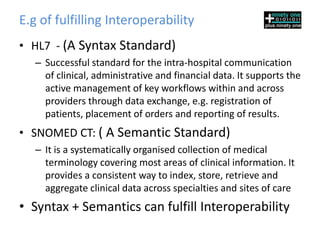
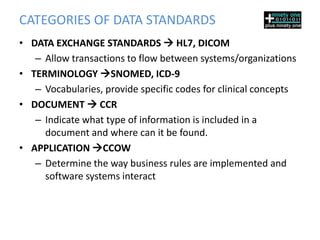
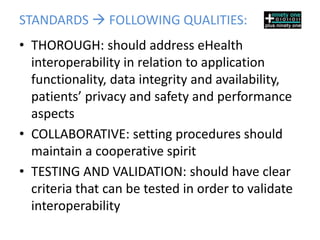
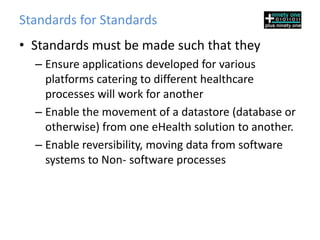
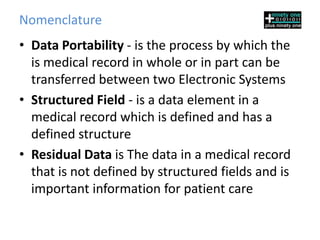
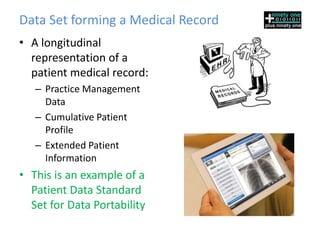
The document discusses clinical data standards and data portability in healthcare. It notes that healthcare needs to better utilize information technologies to improve quality of care, reduce costs, and empower patients. Establishing interoperability between different healthcare systems requires agreed upon data standards to ensure consistent and uniform sharing of information. Examples of data standards that help fulfill interoperability include HL7 for data exchange and SNOMED CT for clinical terminology. Adopting common data standards is key to enabling reliable movement of health information between systems and organizations.