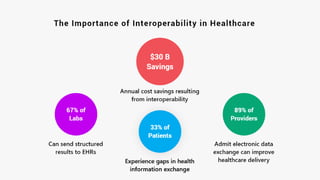
Data interoperability in healthcare enables the seamless exchange and use of electronic information across systems, enhancing patient care and safety. Current challenges in interoperability lead to significant costs, clinician burnout, and compromised patient outcomes, highlighting the need for improved data sharing standards and practices. By embracing interoperability, organizations can enhance efficiency, patient experiences, and the accuracy of public health data, making it a critical focus for the future of healthcare.