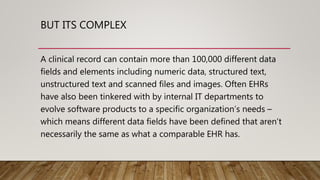
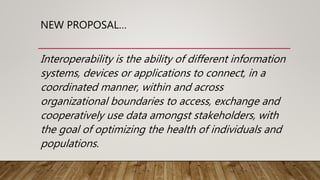
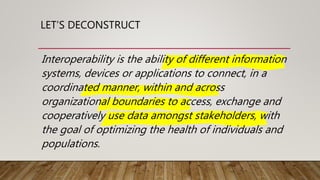
This document summarizes a presentation on interoperability in healthcare. It discusses the current state of interoperability, definitions of interoperability from various organizations, components of interoperability including foundational, structural, semantic and organizational. It also discusses the Fast Healthcare Interoperability Resources (FHIR) standard and reasons for its adoption, as well as ongoing challenges to achieving interoperability in healthcare. In conclusion, the presenter thanks the audience and provides contact information.