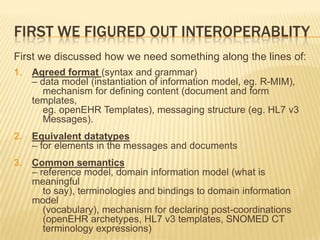
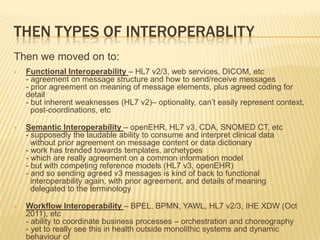
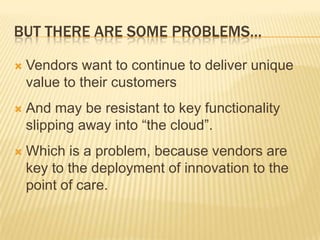
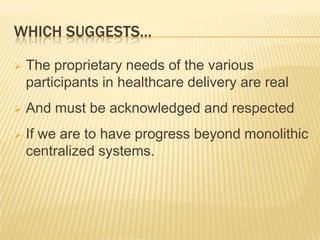
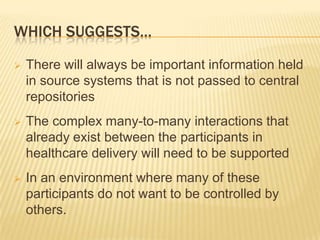
Douglas Kingsford is a practicing GP and CEO who is interested in artificial intelligence, workflow, and electronic health records (EHRs). He discusses that EHRs are about interoperability, sharing data, and collaborating in patient care. However, achieving true interoperability is challenging and requires open standards, clinician input, and good governance. Simply putting data in centralized repositories or expecting everyone to use the same system will not work due to the proprietary needs of various stakeholders and desire for clinicians and patients to control personal data. True interoperability will require new types of cooperation and business models between all involved parties in a distributed system with no central control.