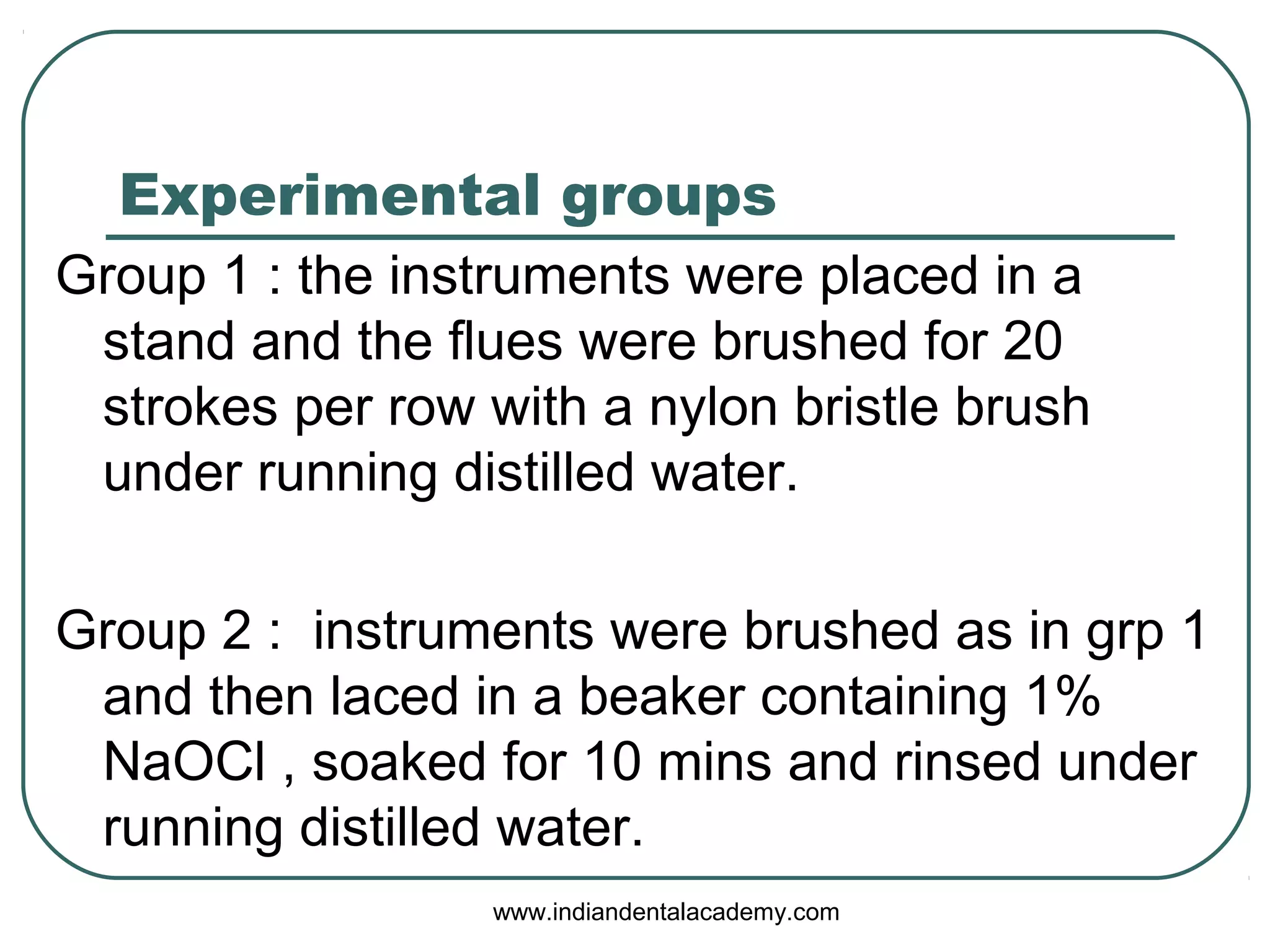
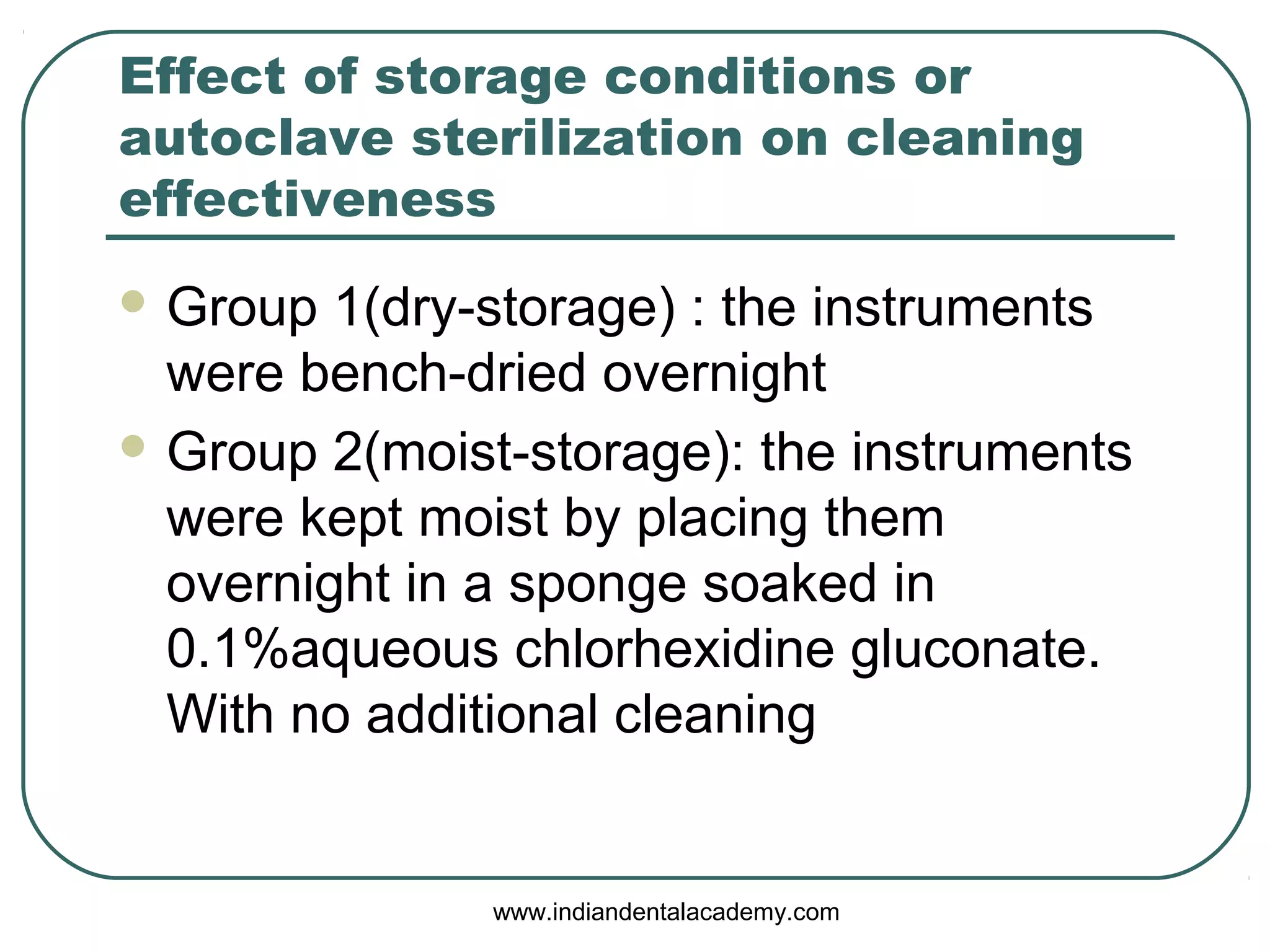
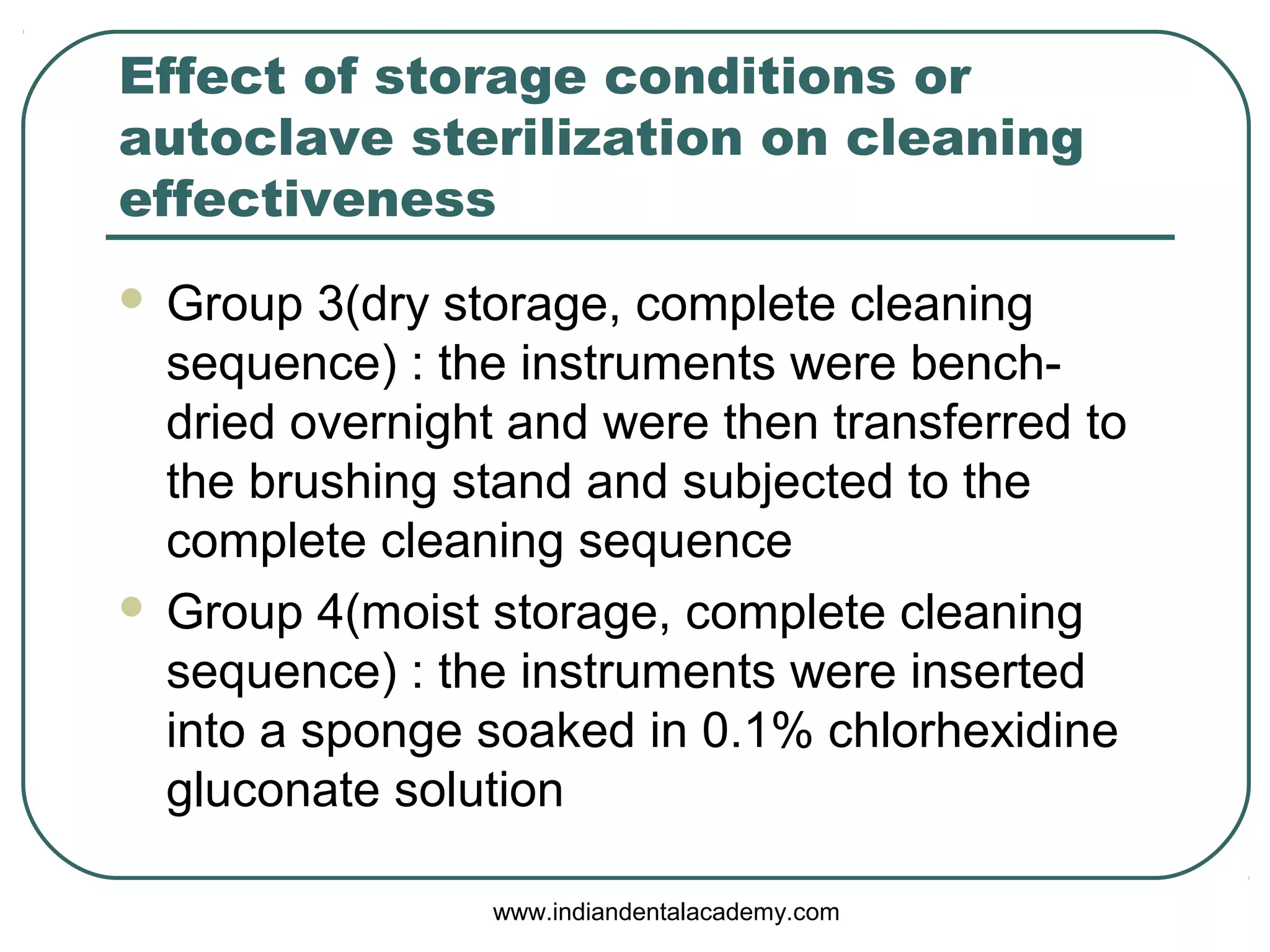
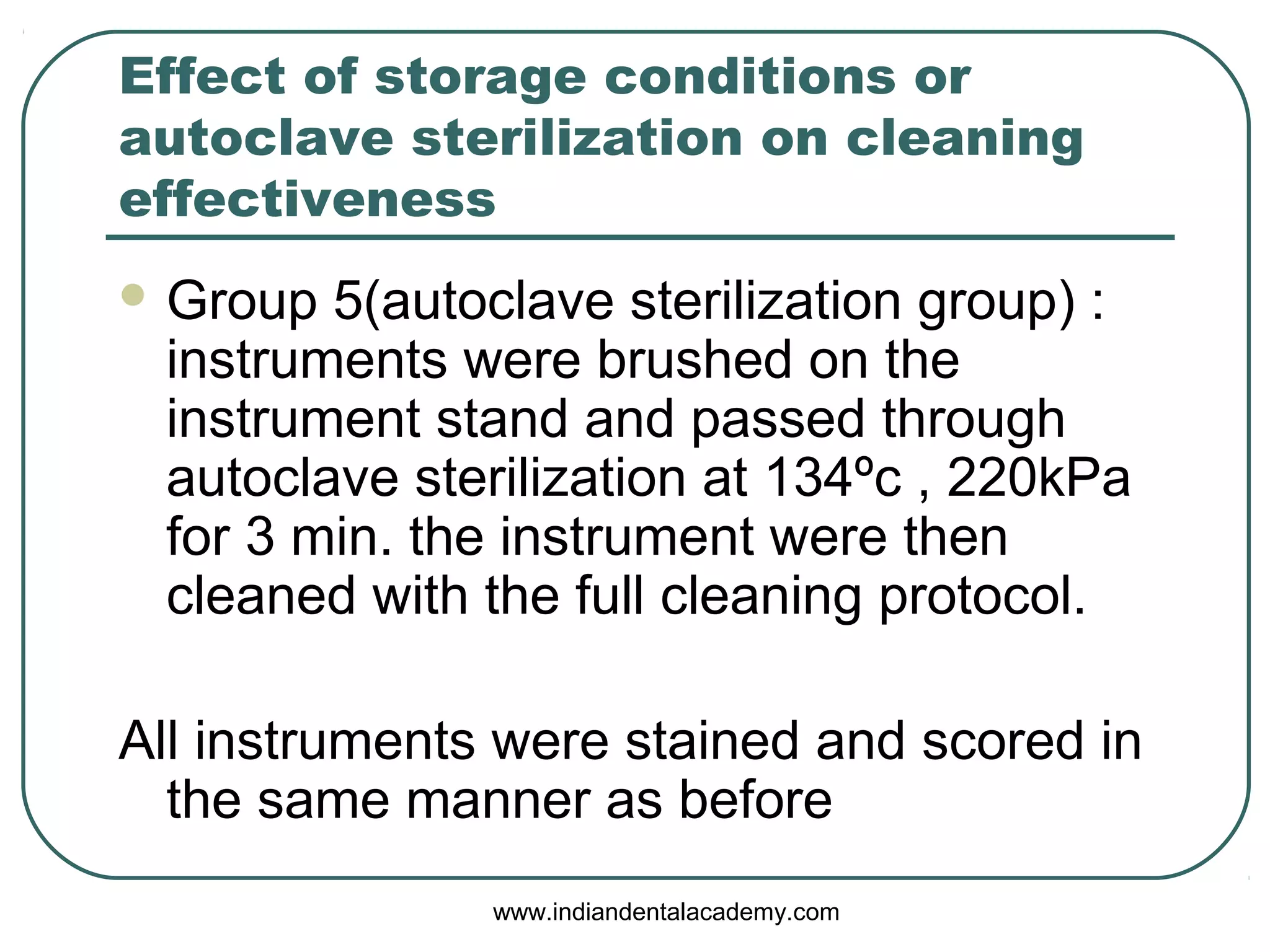
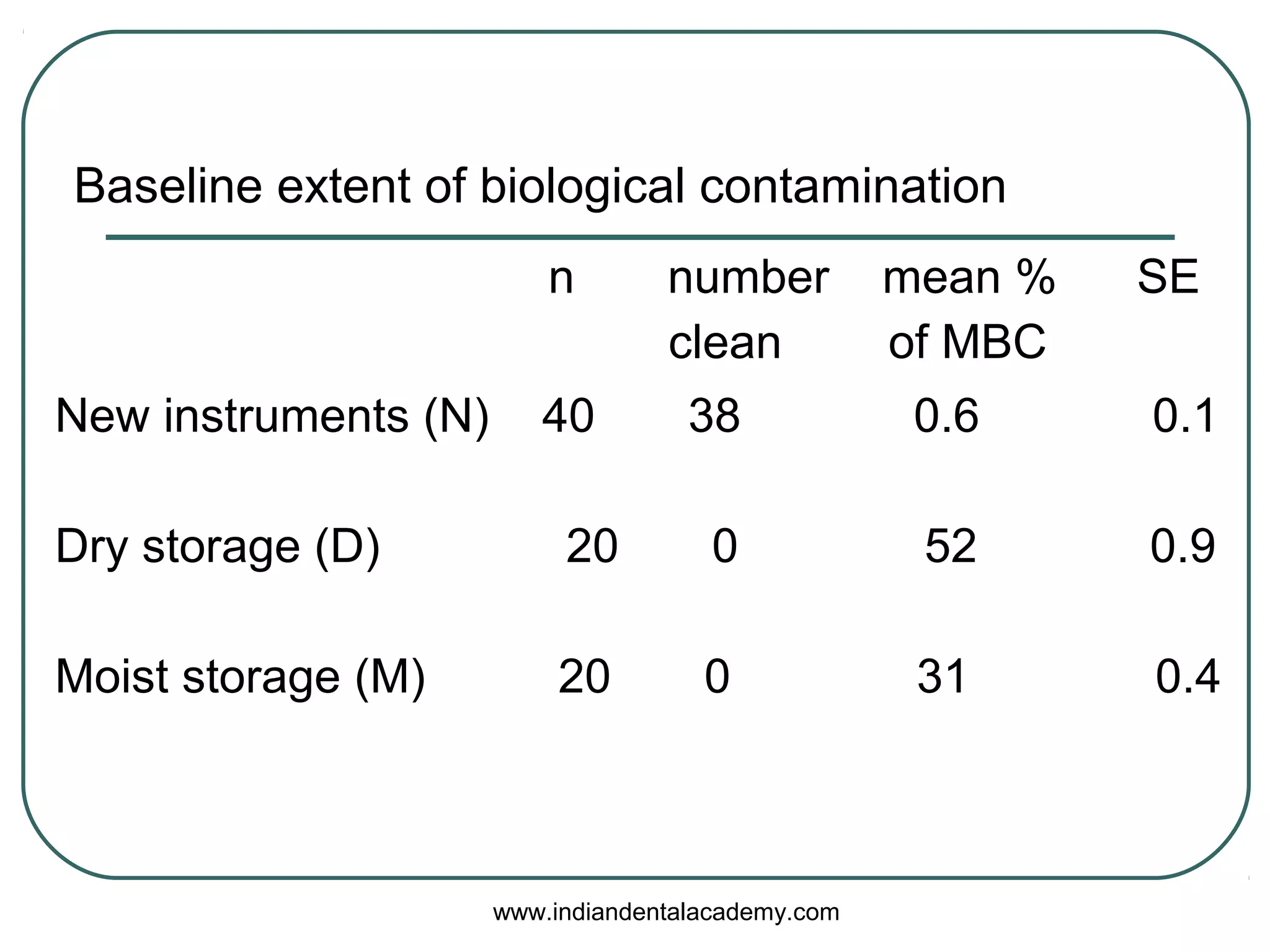
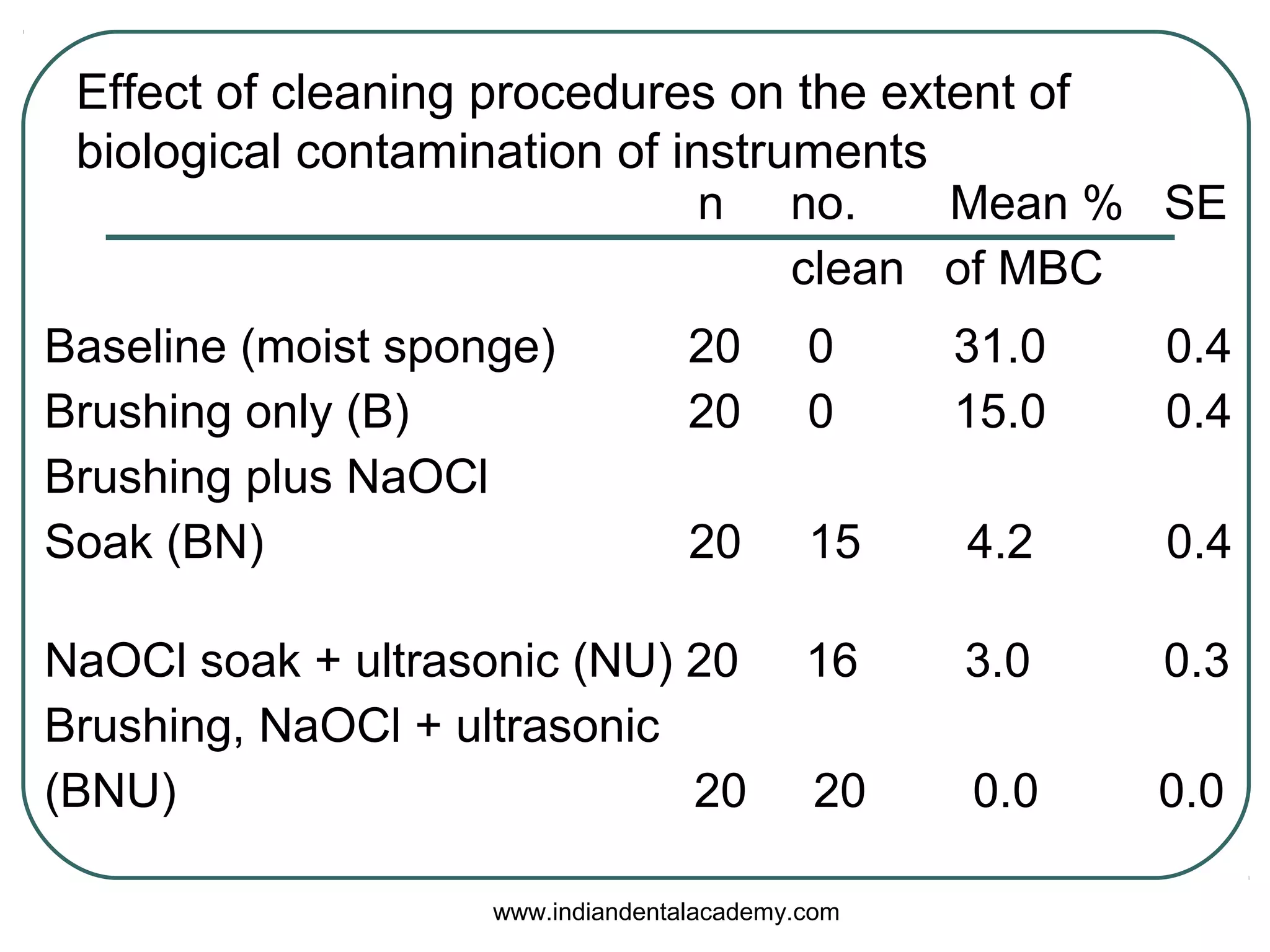
The document discusses the importance of cleaning and sterilizing rotary nickel-titanium endodontic instruments to prevent cross-infection in dental settings. Various sterilization methods, including steam, dry heat, chemical vapors, and ultrasonic baths, are evaluated for their efficacy in removing biological debris. The conclusion emphasizes that no single cleaning method is entirely effective, and a combination of methods is necessary for optimal sterilization.