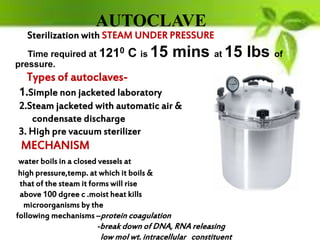
This document provides information on sterilization and infection control in dentistry. It defines key terms like sterilization, disinfection, antisepsis and asepsis. It describes the chain of infection and common routes of disease transmission in a dental office. It discusses various methods of disinfection and sterilization used in dentistry, including heat, chemicals, filtration and radiation. The most common sterilization methods used in dental offices are described as steam autoclaving, chemiclaving and dry heat ovens. The document emphasizes the importance of sterilizing dental instruments according to their risk classification as critical, semi-critical or non-critical to prevent disease transmission.