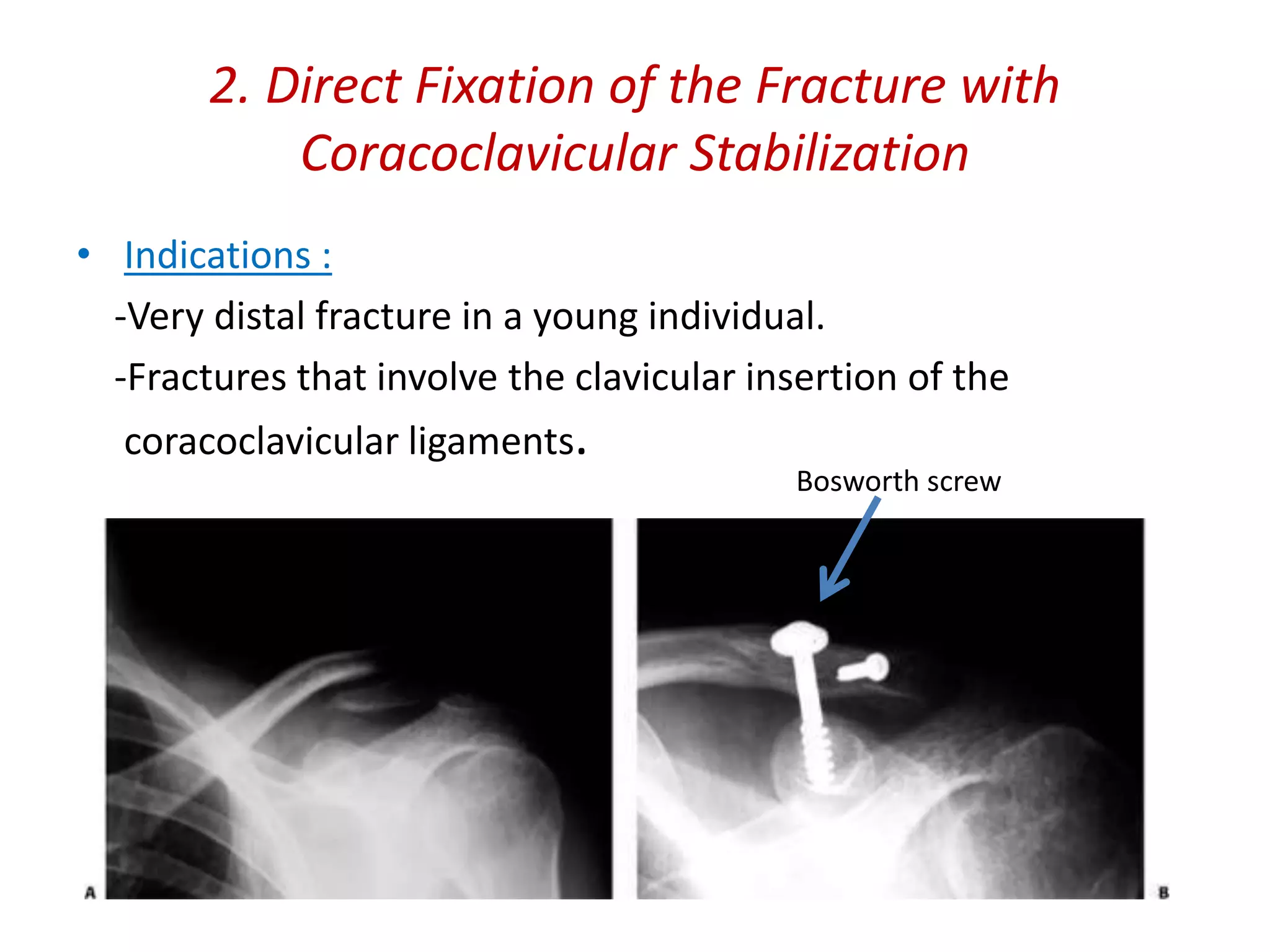
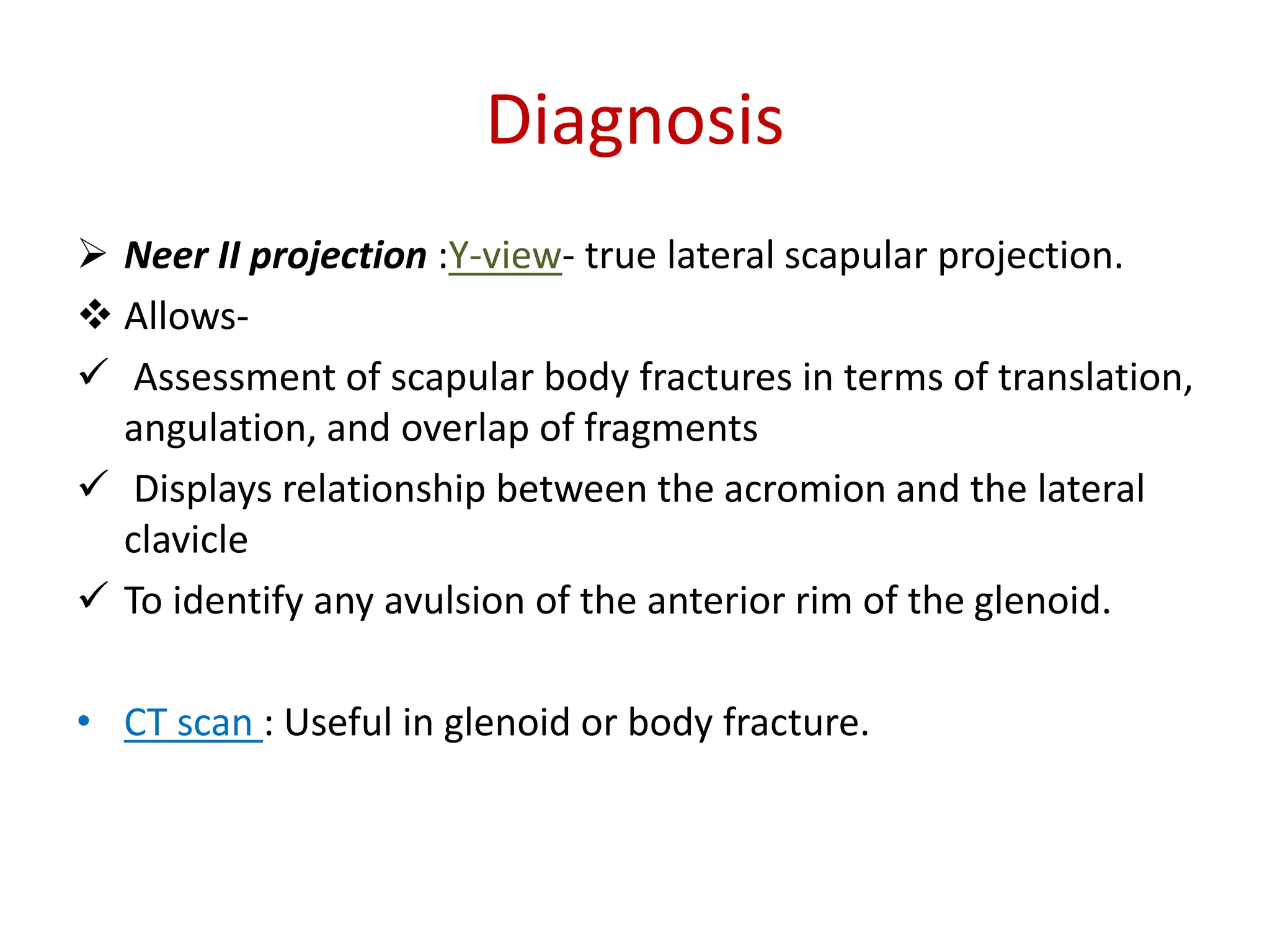
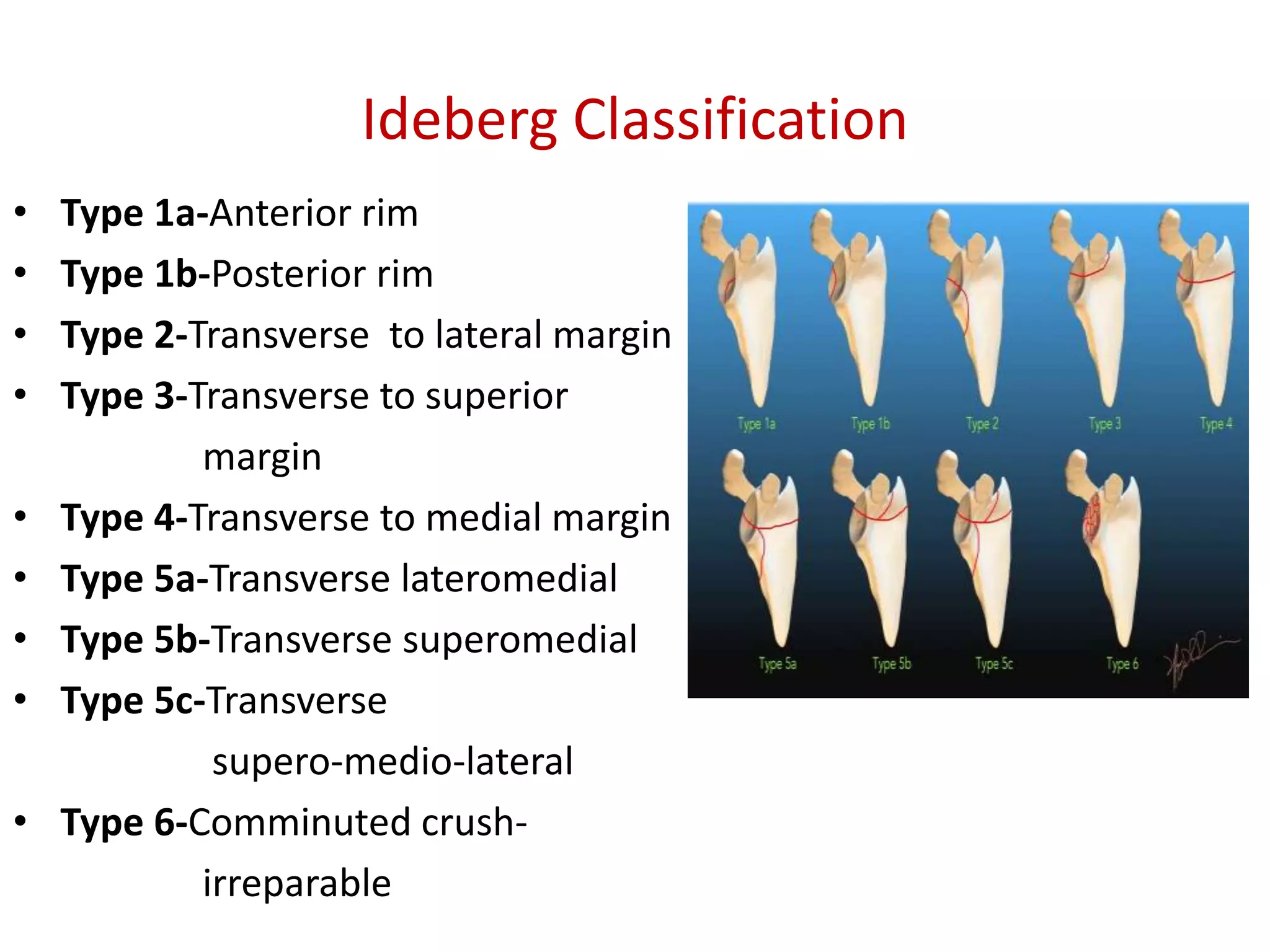
Clavicle and scapular fractures are significant injuries, accounting for a notable percentage of shoulder girdle fractures, with various types and classifications based on their location and displacement. Non-operative treatment is often sufficient for certain types of fractures, while operative options include stabilization techniques for more severe cases, especially when accompanied by complications or associated injuries. Comprehensive evaluation using radiographic techniques is crucial for accurate diagnosis and determining the appropriate treatment plan.







![Classification
Based on the position of the fracture:[“Allman”]
1. Distal third (Group II)
2. Middle third (Group I)
3. Proximal (Group III).
• “Neer” divided distal clavicle fractures into three subgroups,
based on their ligamentous attachments and degree of
displacement.](https://image.slidesharecdn.com/clavicleandscapular-200706114348/75/Clavicle-and-scapular-fracture-8-2048.jpg)