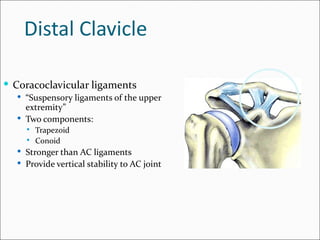
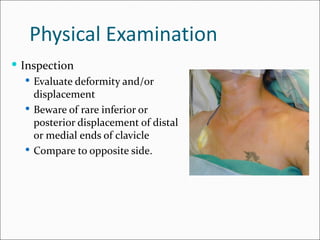
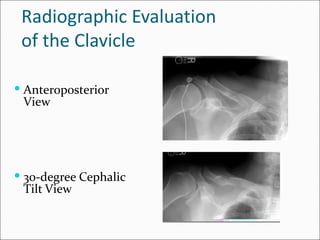
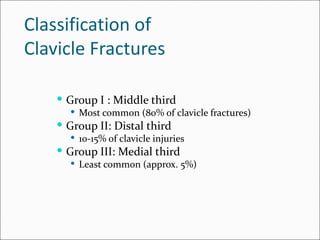
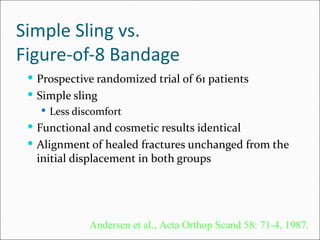
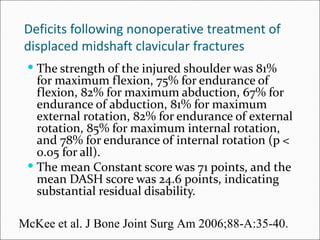
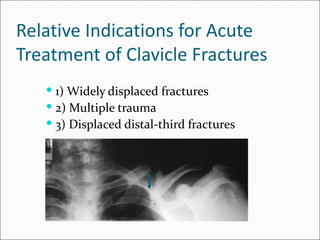
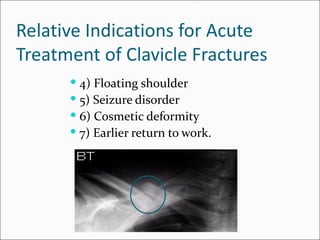
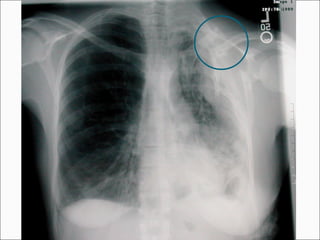
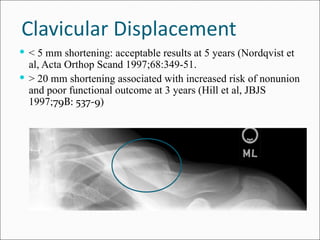
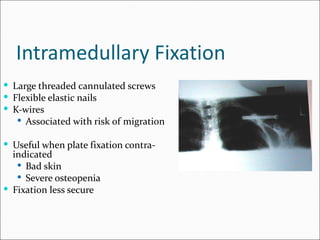
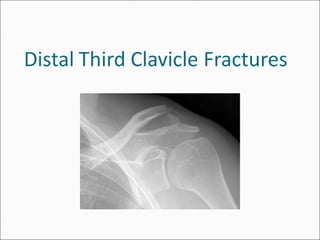
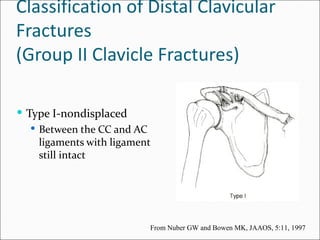
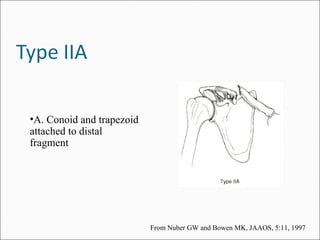
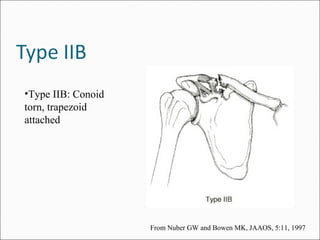
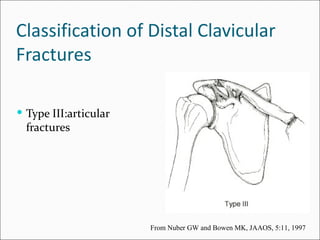
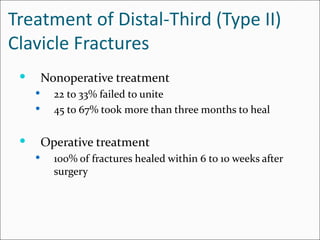
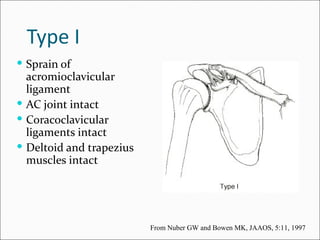
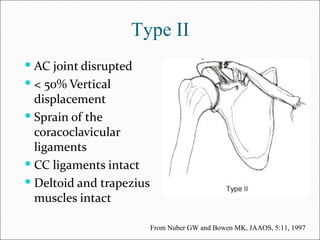
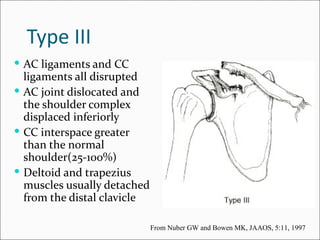
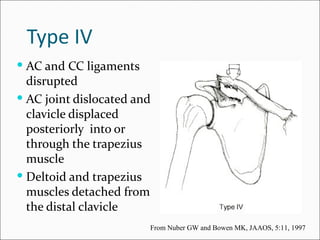
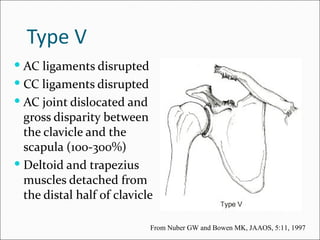
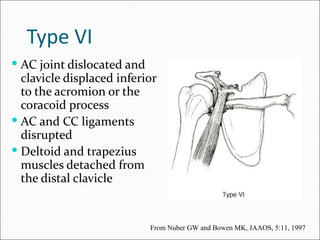
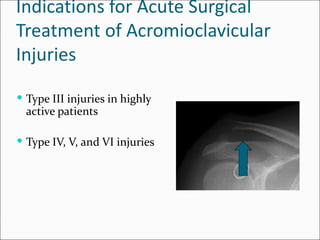
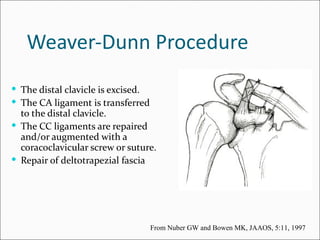
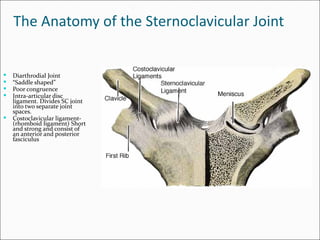
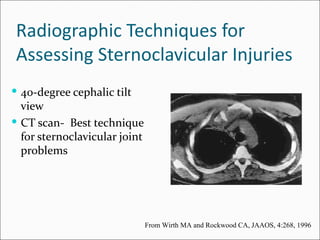
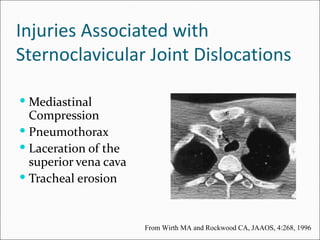
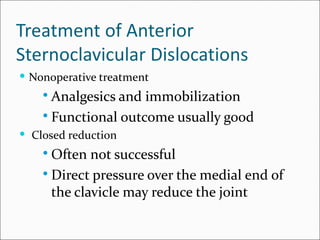
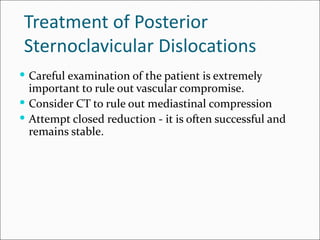
The document describes the anatomy and classification of injuries to the clavicle, acromioclavicular joint, and sternoclavicular joint. It discusses the clavicle bone, its joints, ligaments, muscle attachments, mechanisms of injury, physical exam, radiographic evaluation, classification of fractures, and treatment options for fractures and dislocations which can include nonoperative treatment, plate fixation, intramedullary fixation, coracoclavicular screw fixation, and distal clavicle excision.