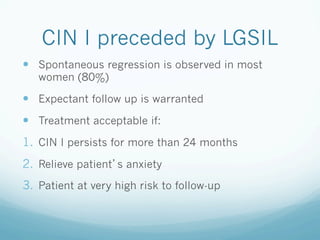
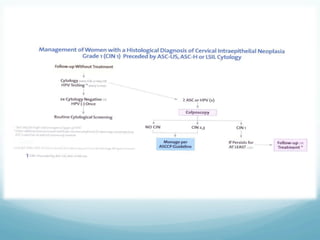
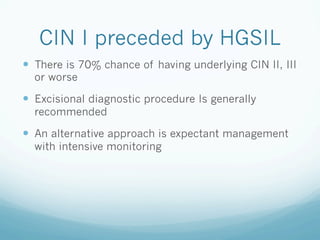
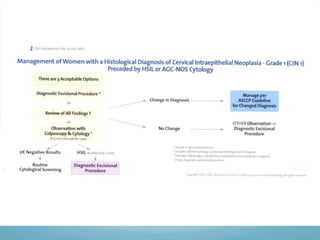
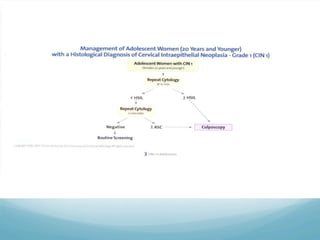
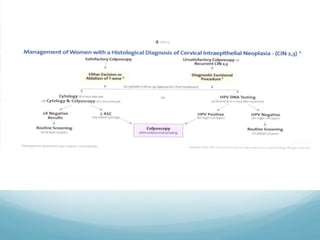
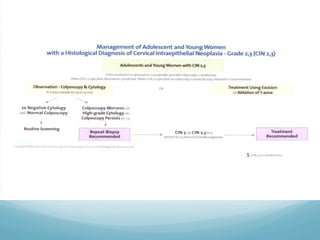
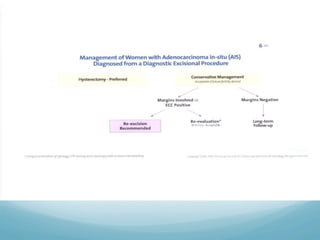
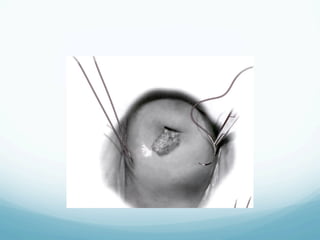
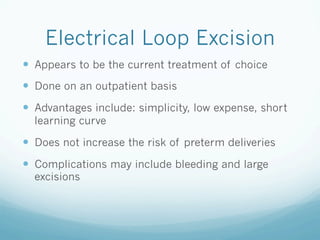
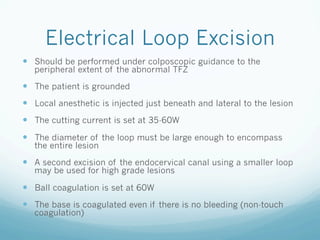
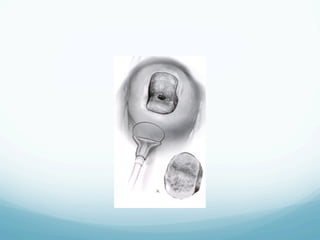
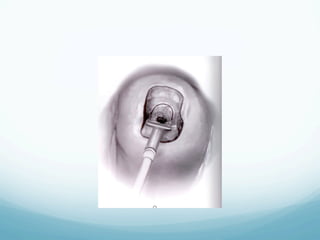
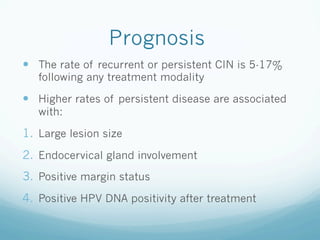
This document discusses the management of cervical intraepithelial neoplasia (CIN). It covers who and when to treat CIN, treatment options including cryotherapy, laser vaporization, loop electrosurgical excision procedure, and conization. It provides guidance on treatment based on CIN grade, patient characteristics like pregnancy, and risk factors. The main treatment goals are prompt treatment of CIN 2-3 while allowing regression of many CIN 1 cases. Complications, reproductive outcomes, and prognosis after treatment are also reviewed.