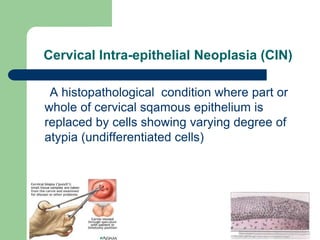
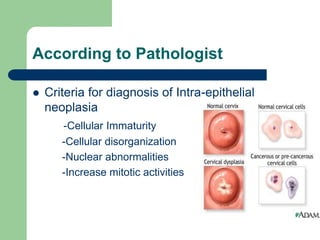
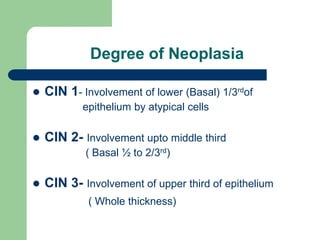
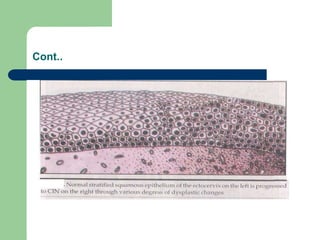
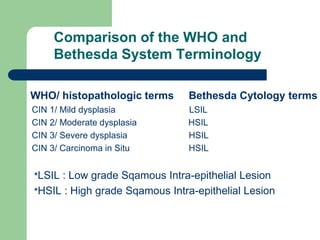
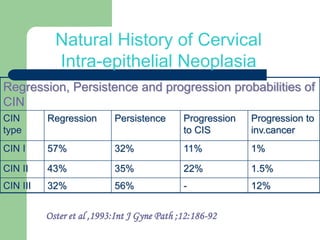
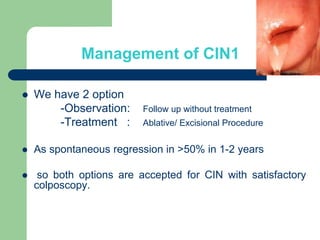
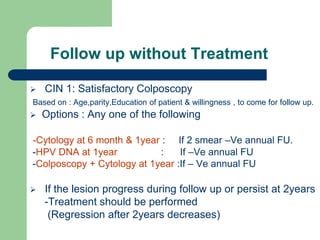
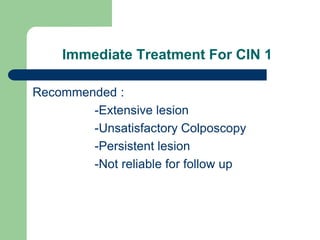
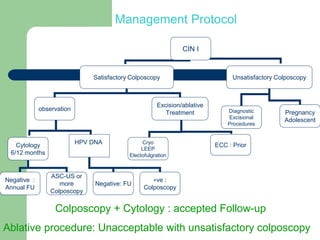
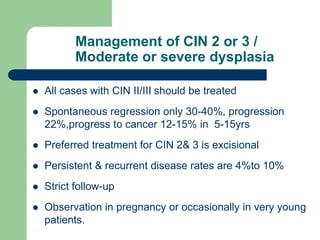
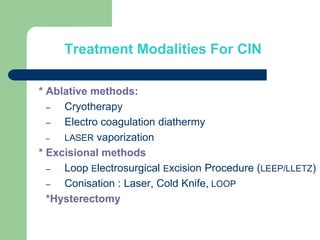
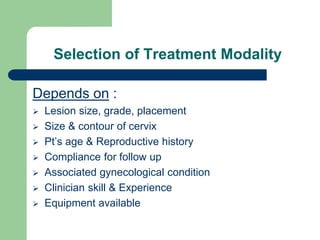
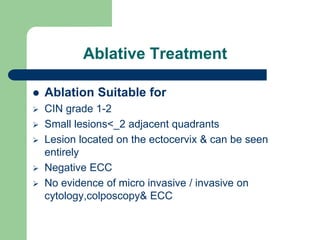
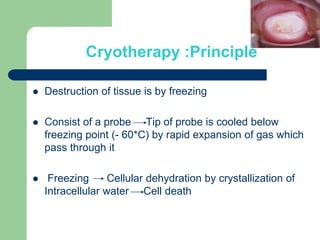
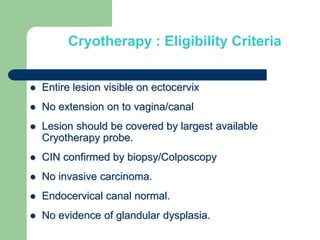
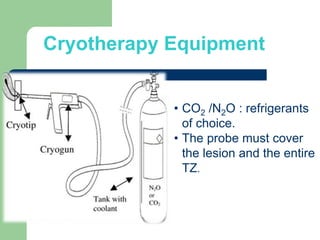
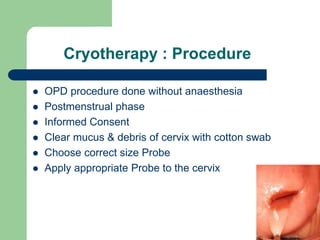
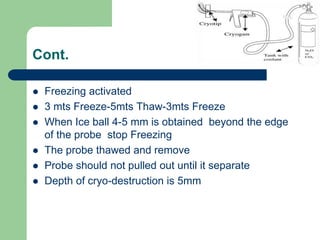
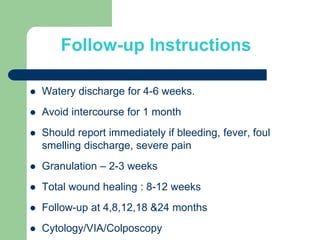
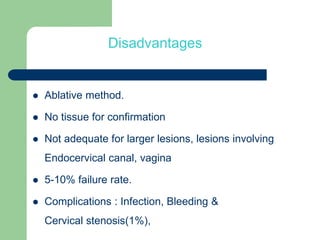
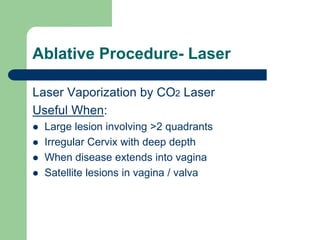
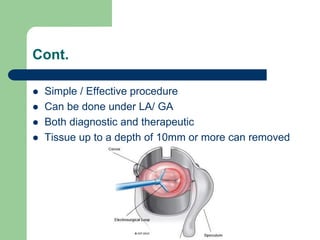
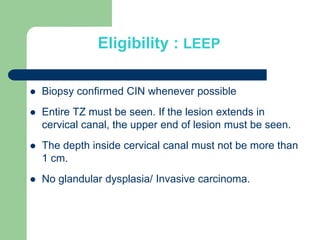
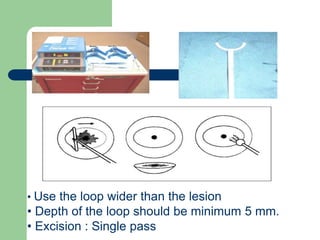
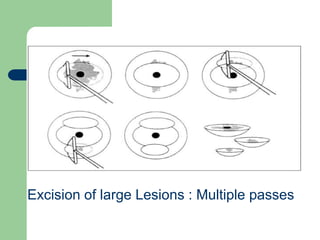
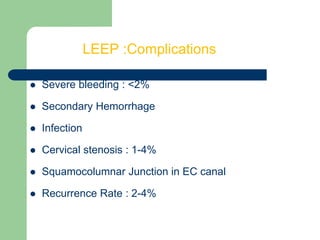
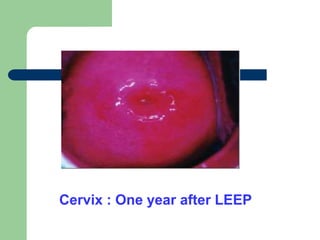
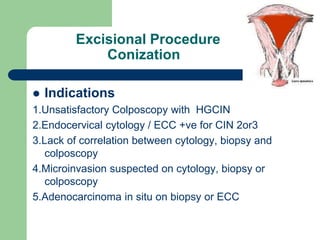
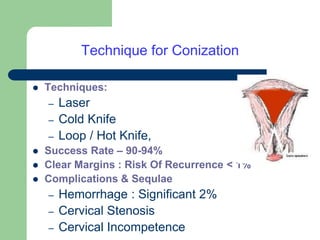
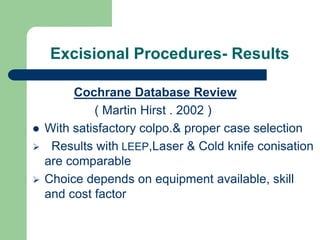
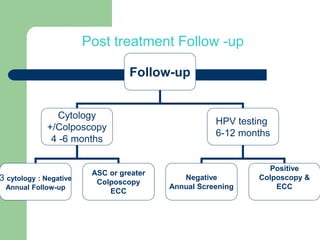
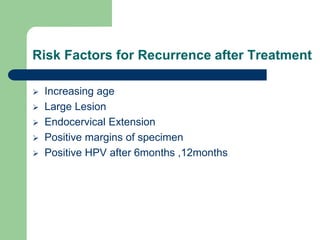
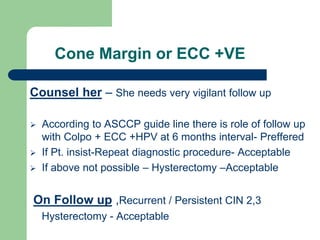
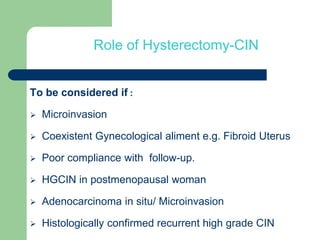
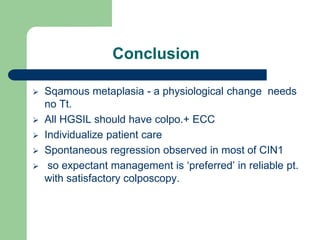
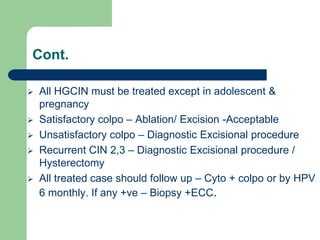
This document discusses the management of cervical intraepithelial neoplasia (CIN). It defines CIN and describes its grading from CIN1 to CIN3 based on the level of involvement of the cervical epithelium. For CIN1, observation or treatment are accepted depending on factors like age and lesion characteristics. CIN2/3 should be treated as regression is only 30-40% and progression risk is higher. Accepted treatment modalities include ablation methods like cryotherapy or laser vaporization and excisional methods like LEEP. Follow up is important after treatment to monitor for regression or recurrence.