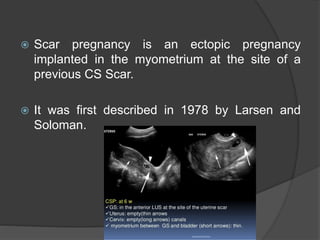
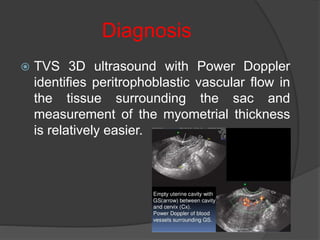
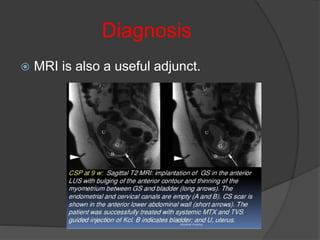
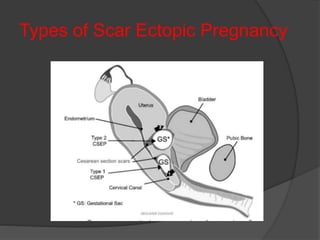
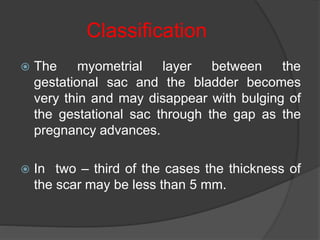
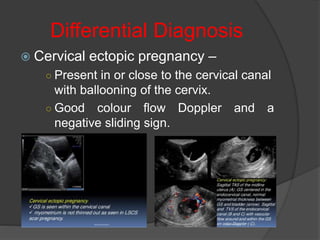
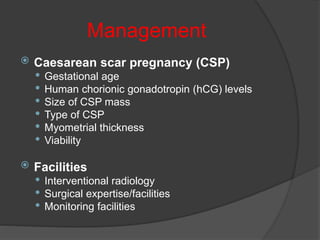
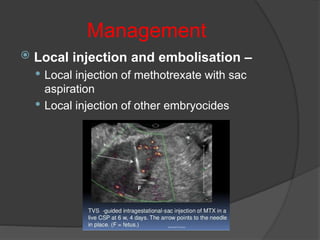
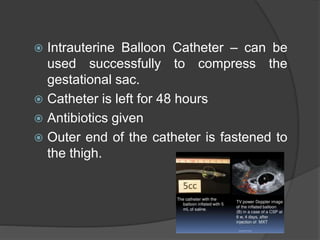
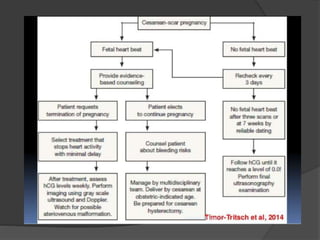
Cesarean scar pregnancy (CSP) occurs when a pregnancy is implanted in the myometrium at the site of a previous cesarean section scar. The risk factors include previous cesarean section, manual removal of placenta, or other uterine trauma. Transvaginal ultrasound is the primary diagnostic tool, showing an empty uterine cavity with the gestational sac embedded in the cesarean section scar. Treatment depends on gestational age, beta-hCG levels, viability, and involves options like expectant management, medical management with methotrexate, surgical evacuation or resection, or hysterectomy in severe cases. Combination treatments are often most effective in terminating the pregnancy while preserving the uterus.