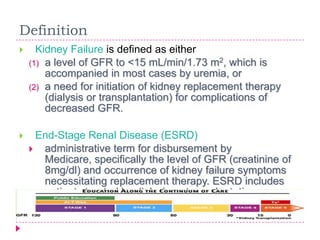
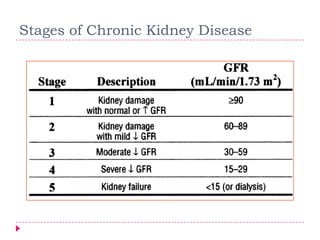
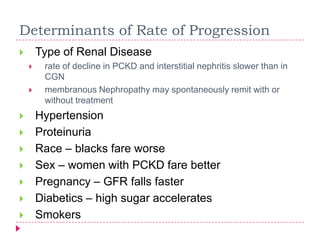
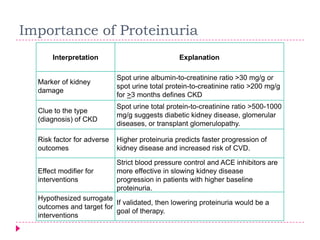
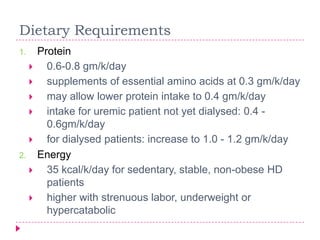
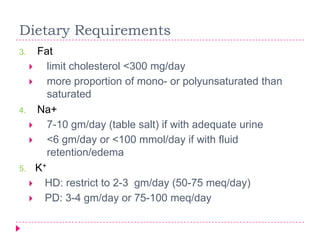
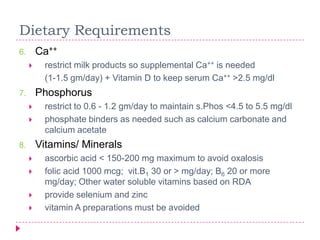
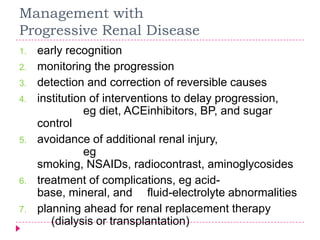
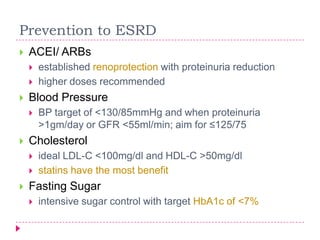
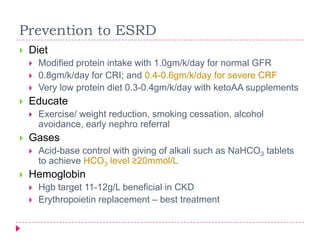
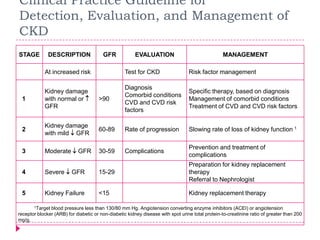
Chronic kidney disease is defined as either kidney damage or decreased glomerular filtration rate (GFR) below 60 mL/min/1.73m2 lasting at least 3 months. The causes of chronic kidney disease include diabetes, hypertension, glomerulonephritis, and polycystic kidney disease. Management involves monitoring progression, treating complications, and planning for renal replacement therapy if kidney failure develops. Preventing progression to end-stage renal disease focuses on tight control of blood pressure, cholesterol, blood sugar, diet, and use of ACE inhibitors.