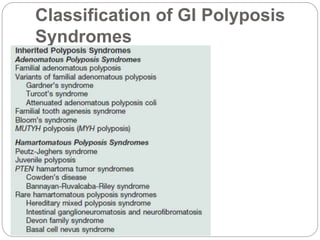
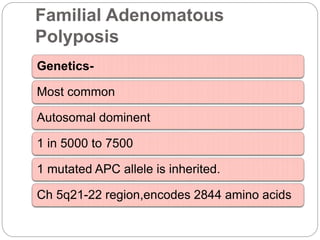
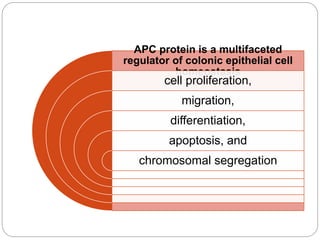
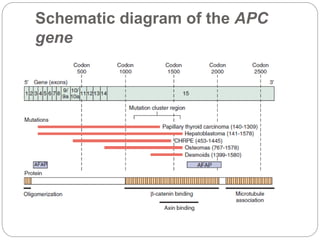
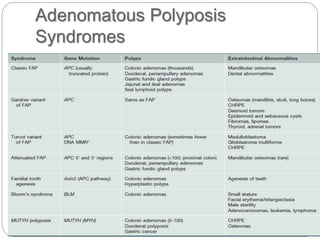
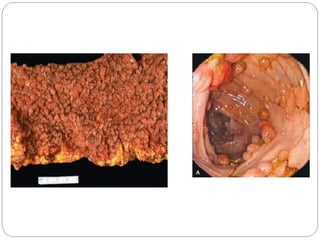
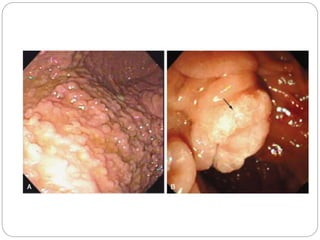
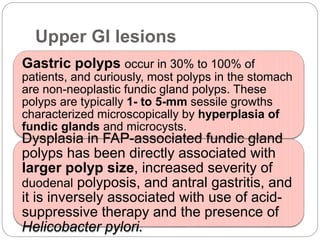
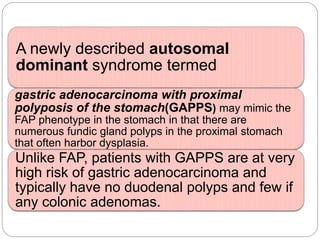
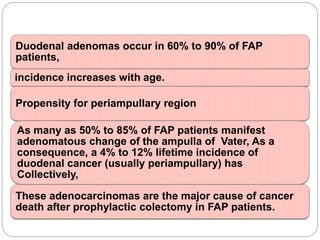
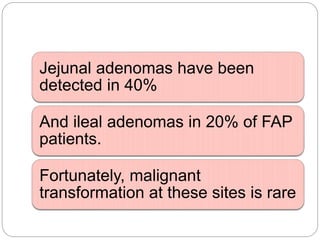
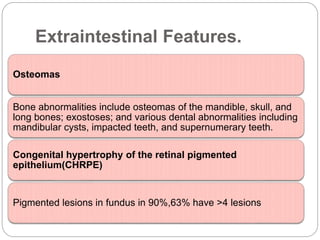
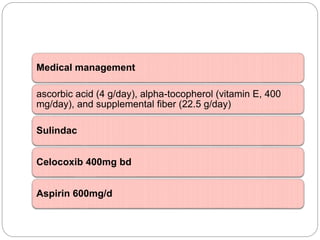
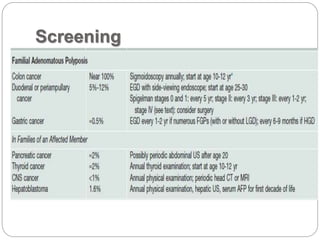
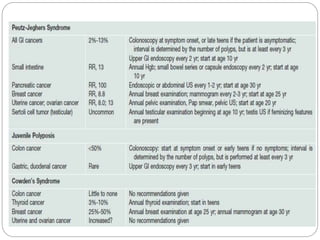
Colonic polyposis refers to numerous polyps throughout the GI tract that are often precancerous. The most common type is familial adenomatous polyposis (FAP), an autosomal dominant condition caused by a mutation in the APC gene. People with FAP develop hundreds to thousands of colon polyps by their mid-30s, and colon cancer is inevitable without surgery to remove the colon. They are also at risk of polyps in the stomach and duodenum that can become cancerous. Treatment involves prophylactic colectomy, surveillance of the upper GI tract, and managing extracolonic manifestations such as osteomas and desmoid tumors.