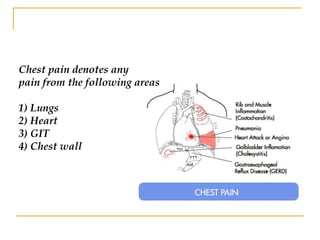
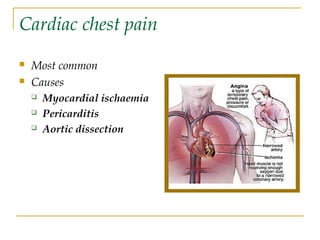
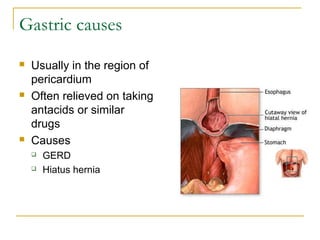
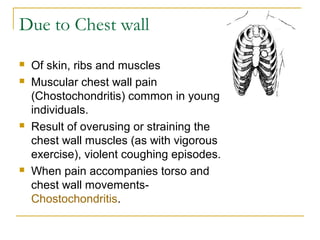
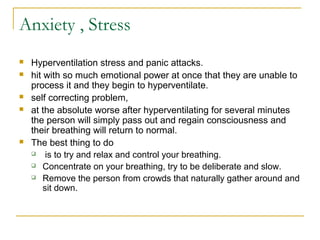
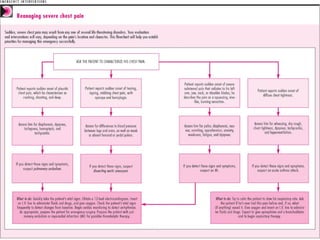
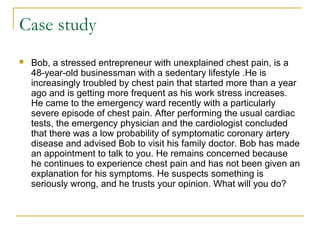
The document discusses various causes of chest pain, categorizing them into cardiac, pulmonary, gastrointestinal, and musculoskeletal sources, with detailed descriptions of symptoms and potential treatments. It highlights a case study of a stressed entrepreneur, Bob, whose chest pain was identified as atypical GERD symptoms after thorough cardiac examinations, leading to effective management with a PPI. The document emphasizes the importance of careful diagnosis and management of chest pain to alleviate patient anxiety and improve health outcomes.