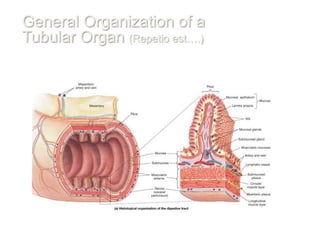
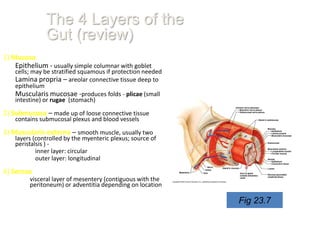
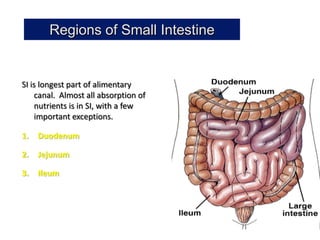
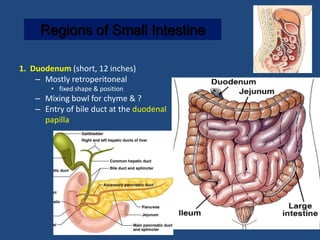
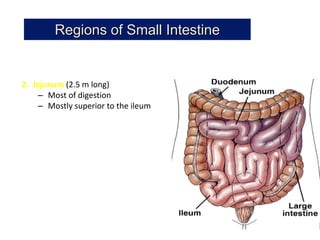
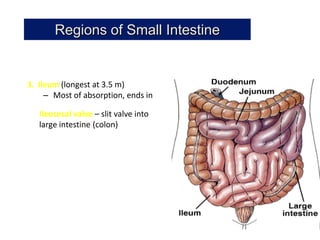
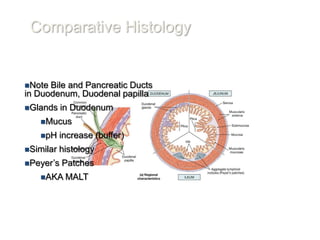
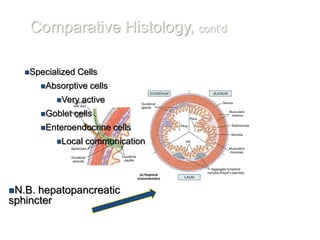
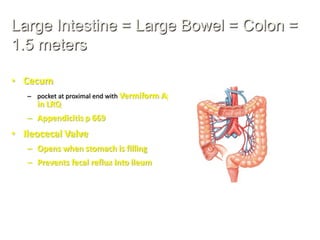
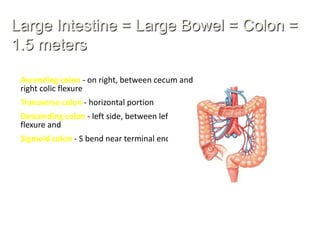
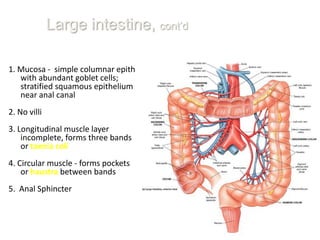
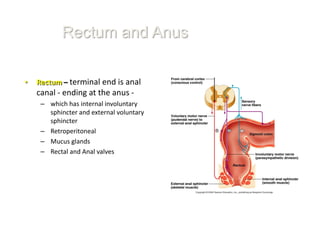
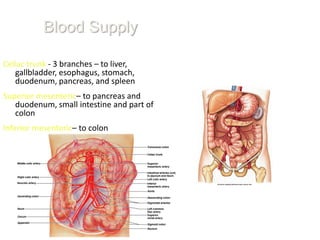
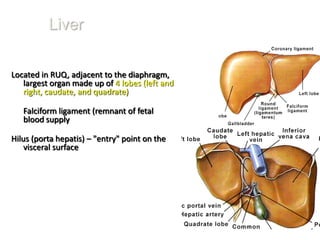
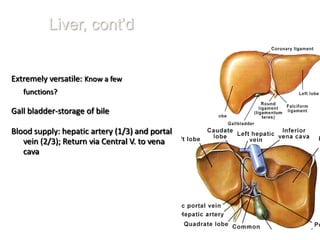
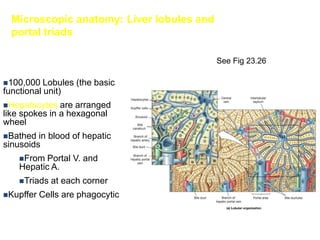
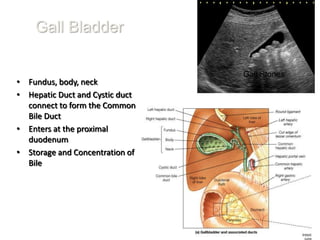
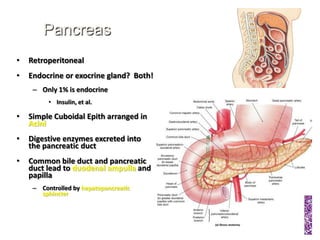
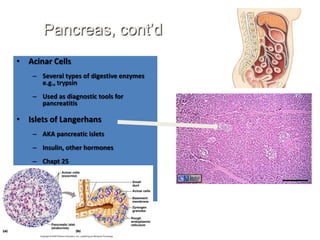
The document discusses the anatomy and functions of the digestive system, describing the tubular nature of the digestive tract and its individual organs like the liver, gallbladder, pancreas, and sections of the small and large intestines. It provides details on the histology and microscopic structure of the digestive organs and discusses their roles in digestion and absorption of nutrients. The major blood vessels supplying the digestive system and regions like the duodenum, jejunum and ileum of the small intestine are also outlined.