Humans
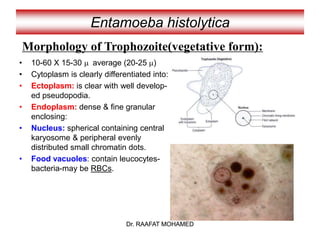
- Trophozoites: 10-30 μm, pear-shaped or rounded with broad blunt pseudopodia
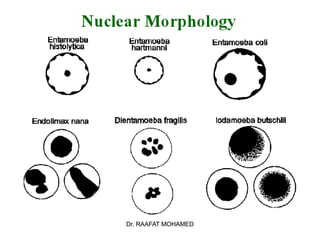
- Nucleus: single, central or subcentral, coarsely granular chromatin
- Feeds on bacteria and debris in mouth
- Cysts: spherical, 8 nuclei, 15-25 μm in size
- Non-pathogenic
- Transmission: direct contact
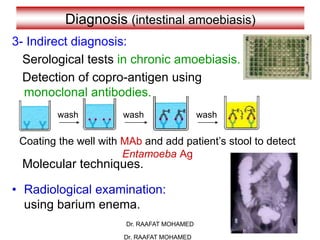
- Diagnosis: finding trophozoites or cysts in dental plaque or gingival scrapings