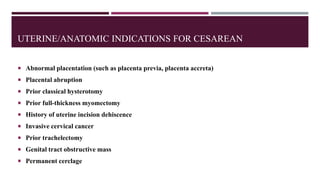
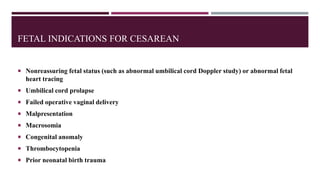
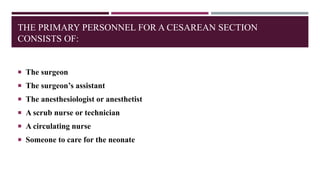
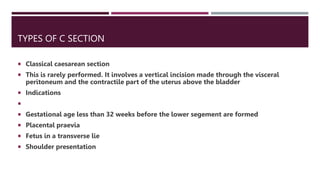
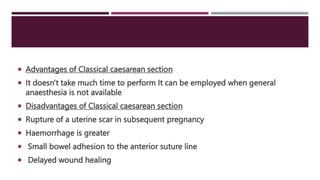
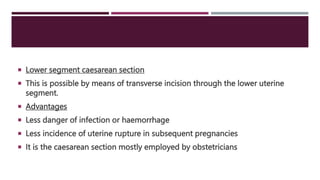
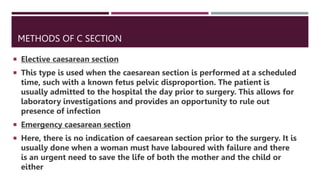
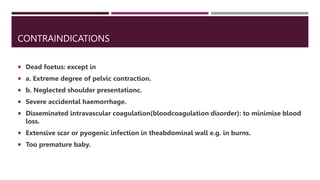
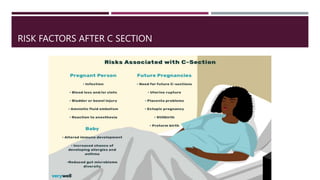
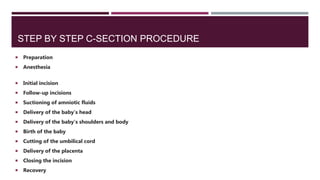
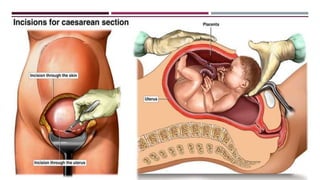
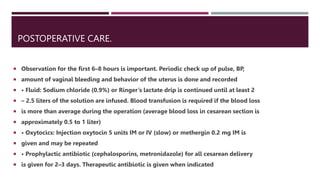
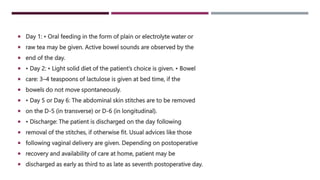
This document provides an overview of cesarean section (C-section). It defines a C-section as a surgical procedure to deliver babies through incisions in the abdominal and uterine walls after 28 weeks of gestation. The C-section rate in the US has risen from 5% in 1970 to 31.9% in 2016. While it poses risks, C-section can be the safest delivery method for some women and babies. The document then describes the personnel, procedures, types, indications, risks, and postoperative care of C-sections.