This document provides information about postpartum hemorrhage (PPH), including its definition, causes, risk factors, prevention, assessment, management, and treatment. Some key points:
- PPH is a leading cause of maternal mortality worldwide, responsible for 1/3 of maternal deaths. The majority occur within 4 hours of delivery.
- Causes (4 Ts) include uterine atony (80% of cases), retained placenta or clots, genital tract trauma, and coagulation disorders.
- Risk factors include overdistended uterus, rapid/prolonged labor, uterine anomalies, and coagulation disorders.
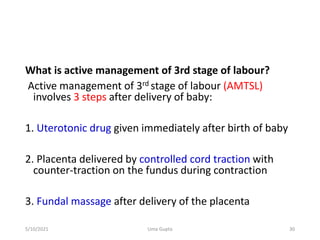
- Prevention is through active management of the third stage of labor