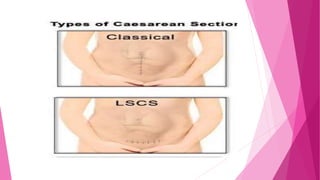
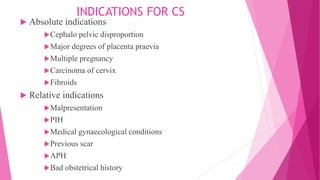
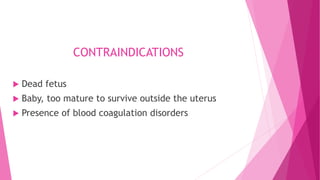
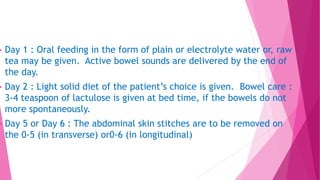
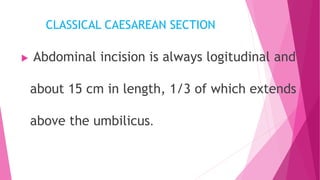
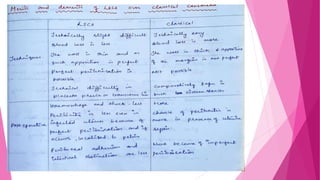
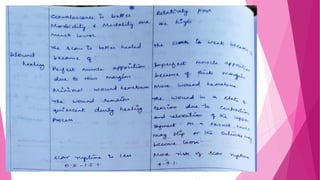
This document discusses Caesarean section, including its definition as delivering a fetus through an incision in the abdominal and uterine walls after 28 weeks of gestation. It lists factors contributing to rising C-section rates and types of operations. Absolute and relative indications for C-sections are provided. The document describes the procedure, management, postoperative care, complications, classical C-section, and caesarean hysterectomy.