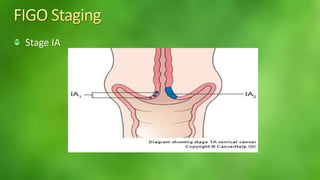
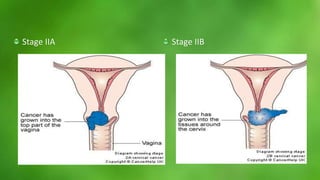
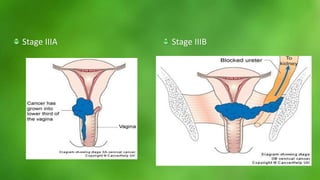
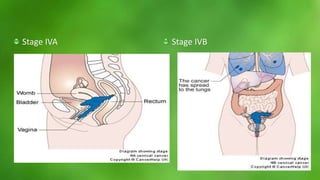
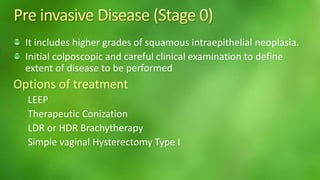
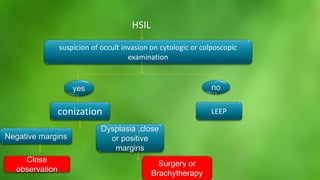
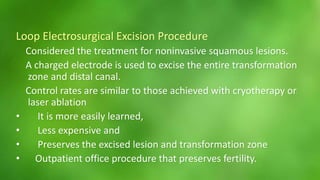
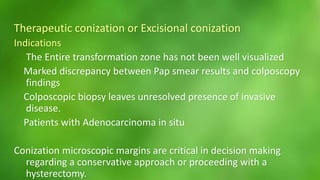
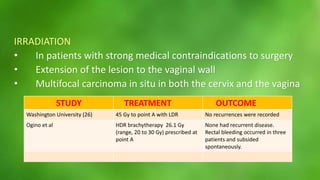
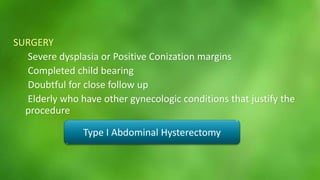
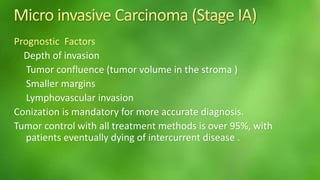
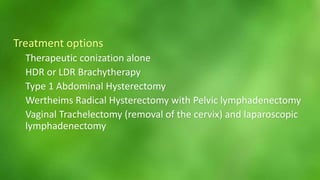
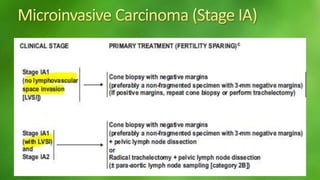
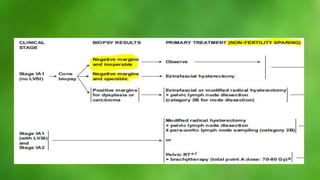
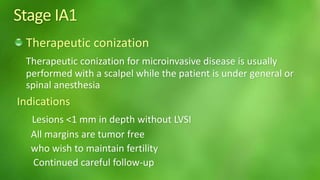
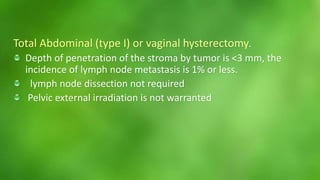
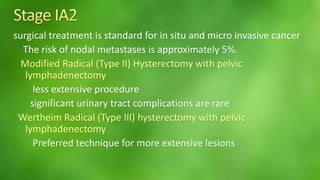
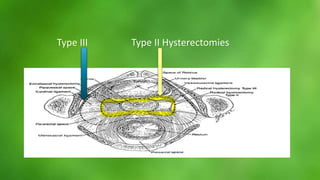
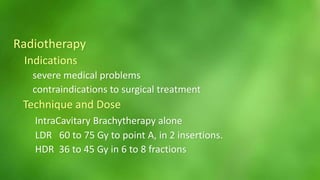
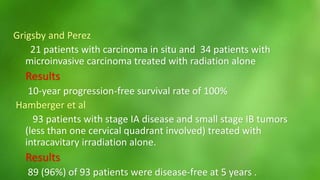
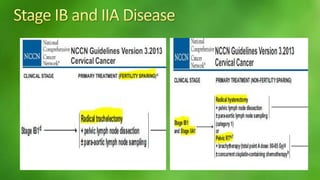
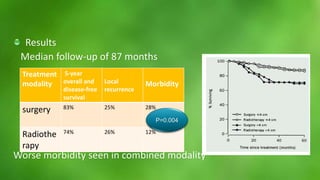
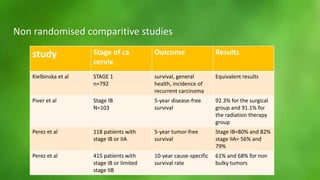
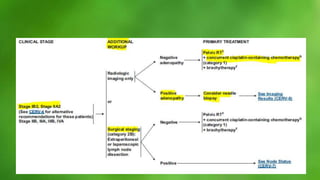
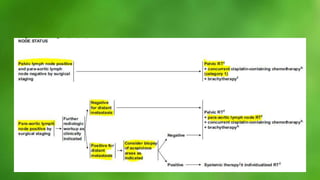
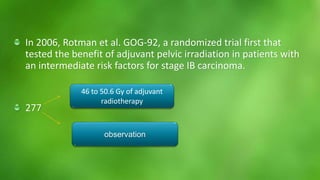
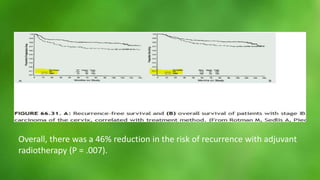
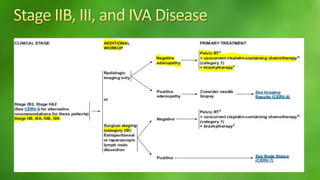
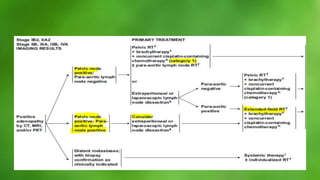
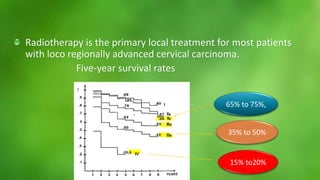
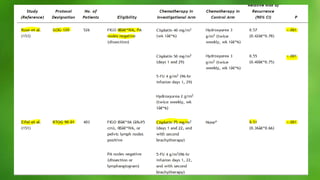
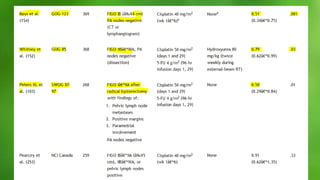
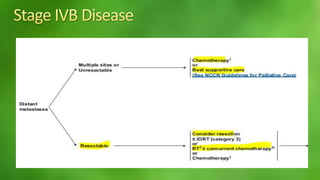
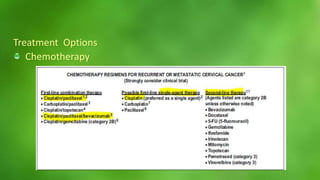
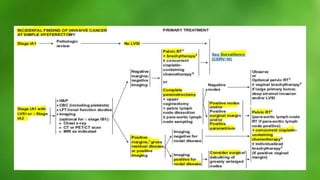
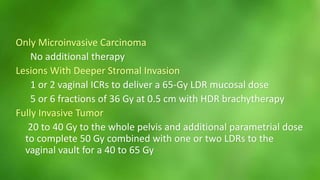
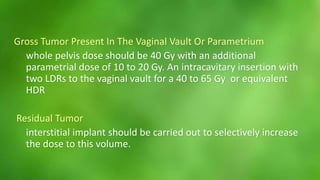
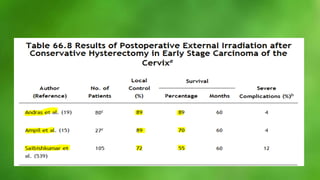
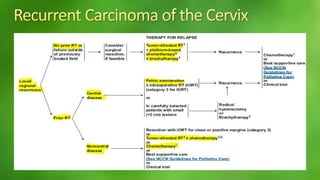
This document discusses staging and treatment options for cervical cancer. It covers stages IA through IVB and describes the diagnostic workup, factors influencing treatment choice, and standard treatment approaches for each stage, including loop electrosurgical excision, conization, brachytherapy, hysterectomy, and radiotherapy. For early stages, options may include close observation, LEEP, conization, or hysterectomy. More advanced stages often receive combinations of chemotherapy, external beam radiation, and brachytherapy. Treatment aims to control the cancer while limiting complications based on each patient's situation.