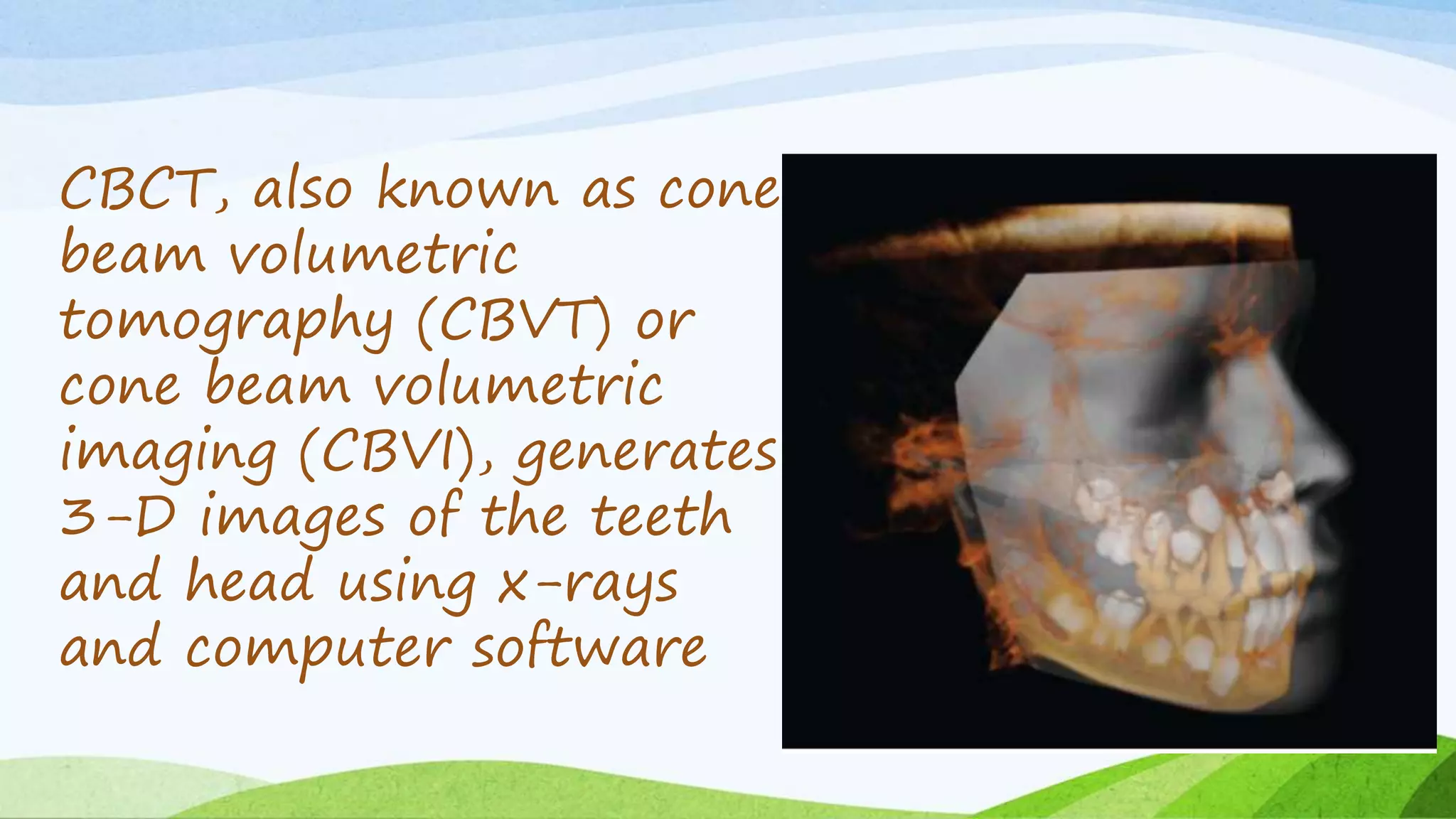
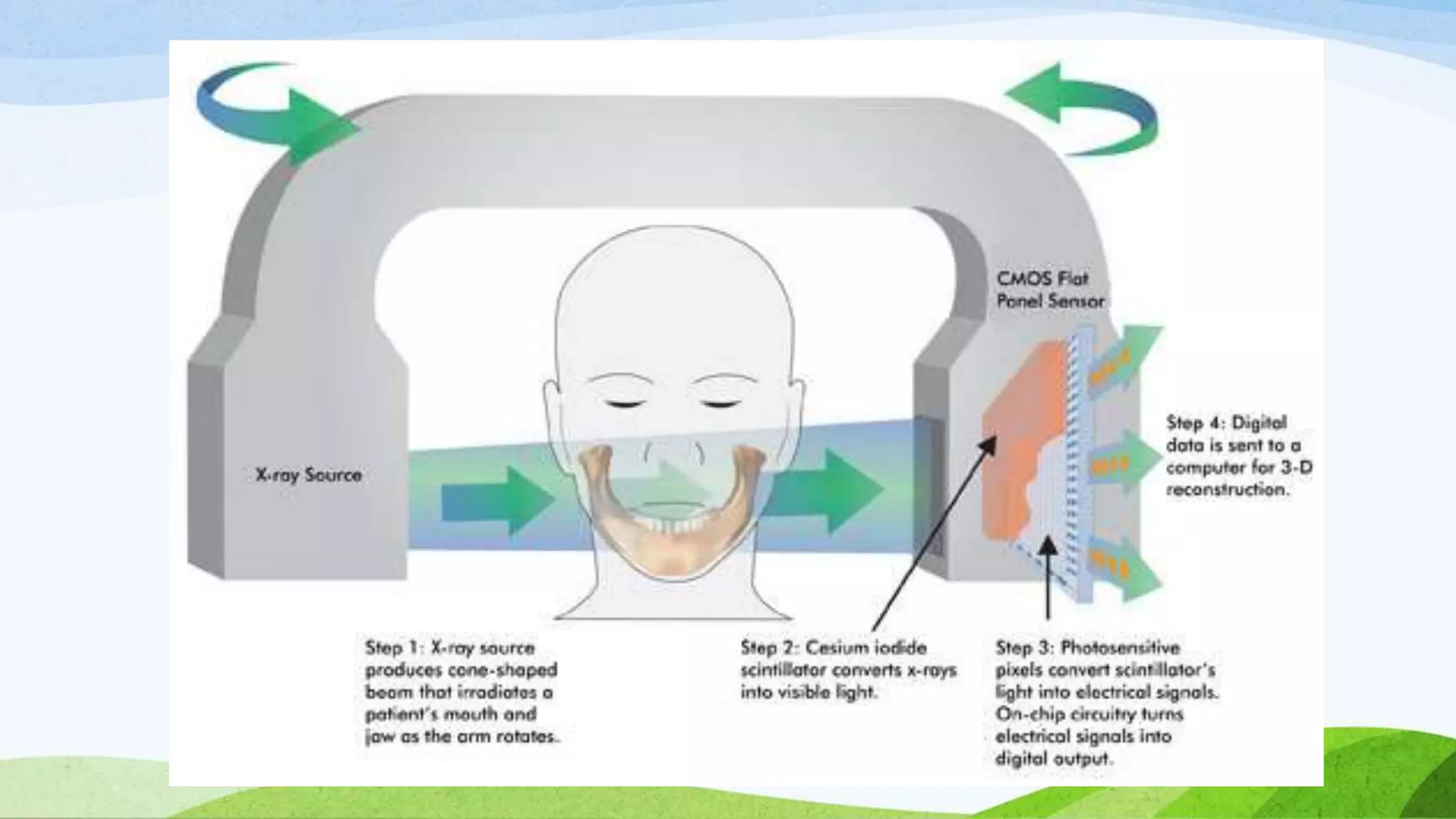
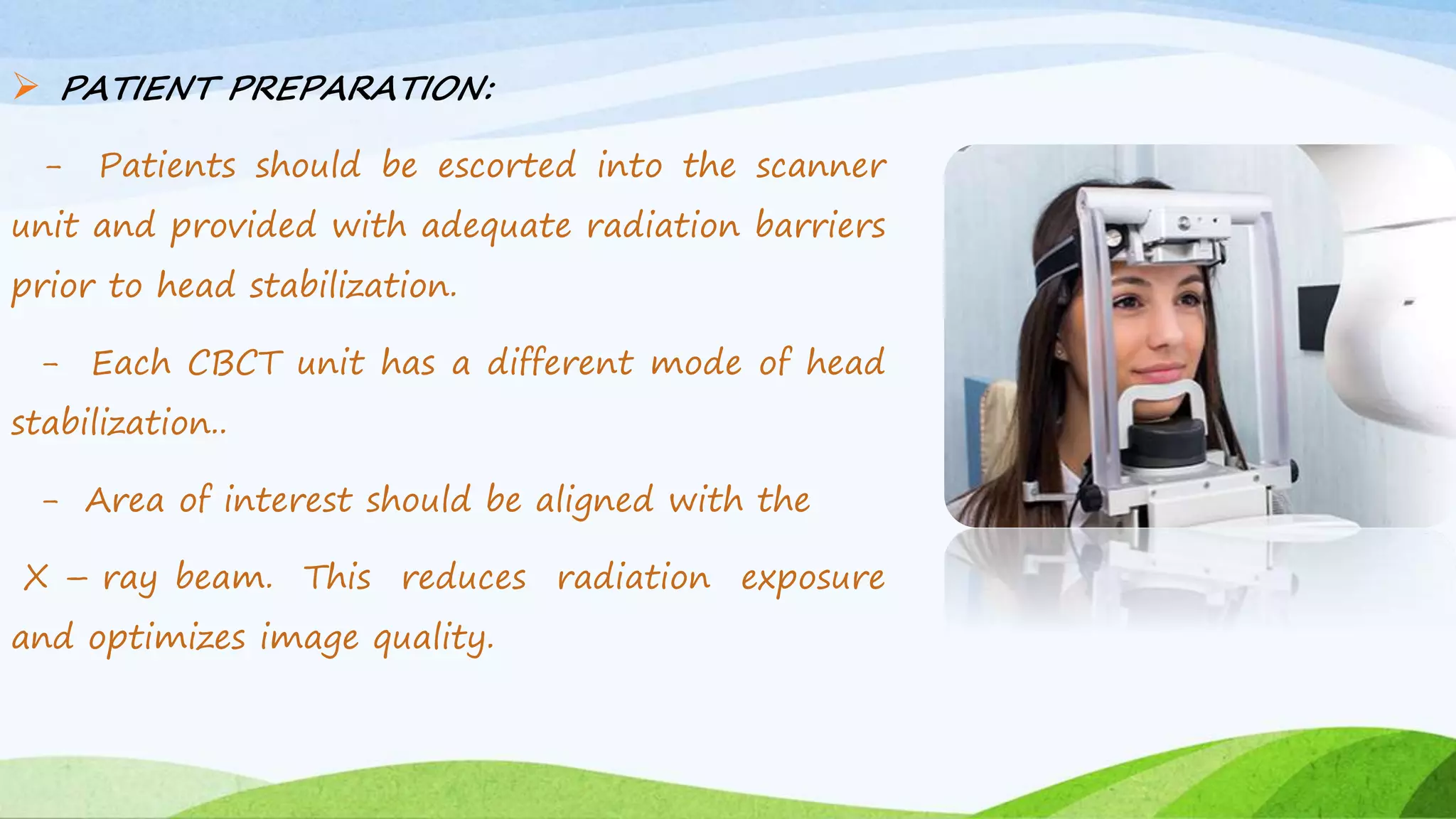
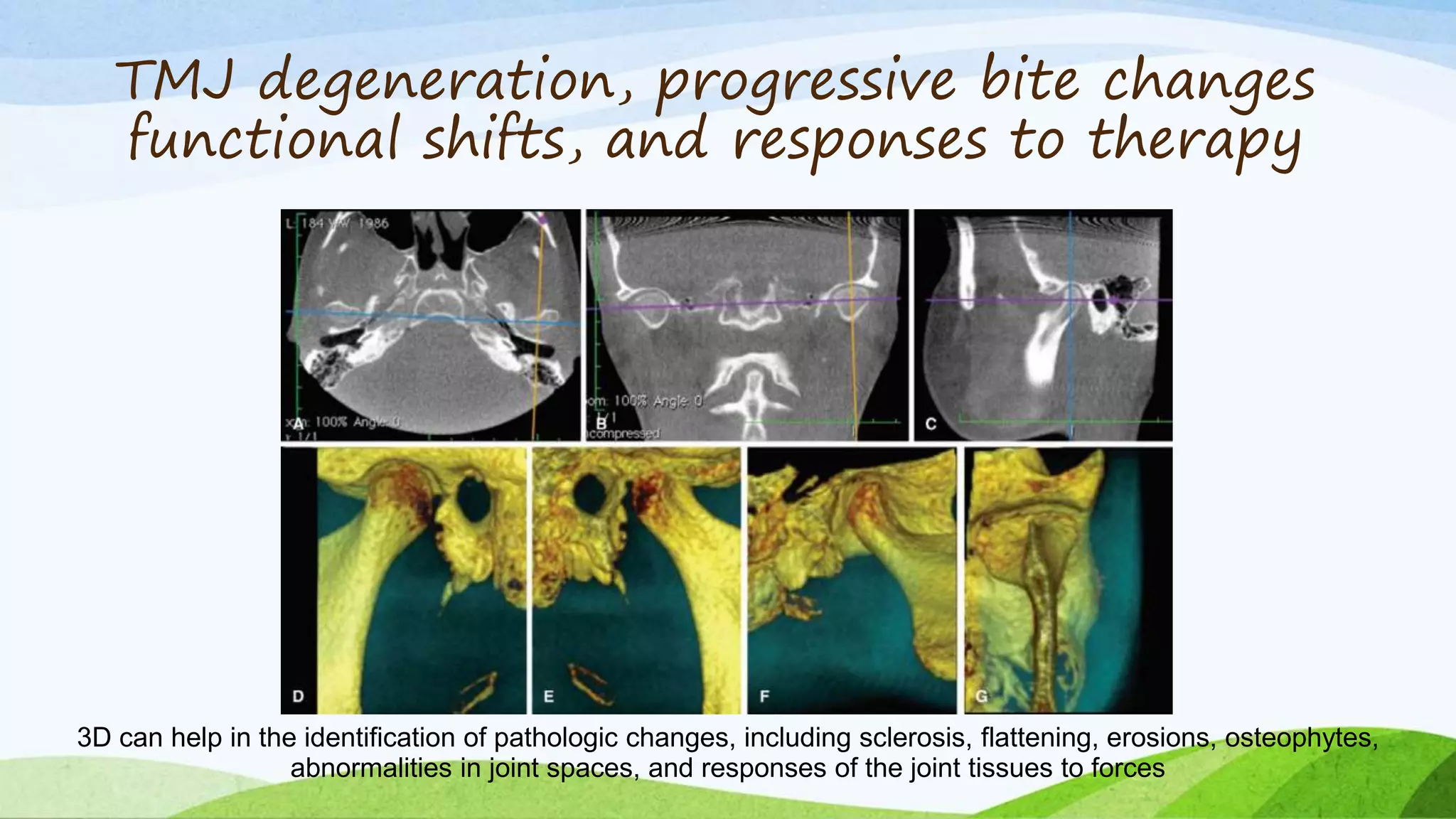
The document discusses Cone Beam Computed Tomography (CBCT) in orthodontics, highlighting its advantages over conventional X-ray imaging, including rapid and painless 3D imaging capabilities. CBCT offers detailed views of facial structures and assists in various applications such as implant site assessment, diagnosing temporomandibular joint issues, and surgical planning. The conclusion emphasizes that CBCT has transformed dental imaging by providing accurate, high-resolution images at lower radiation doses and costs.