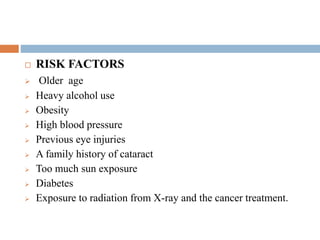
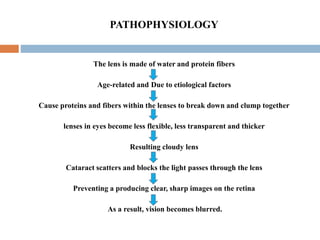
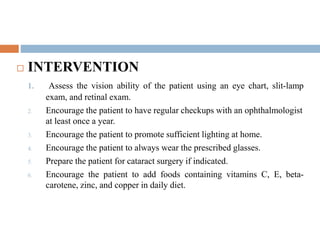
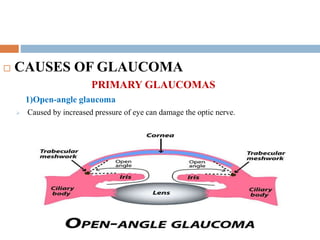
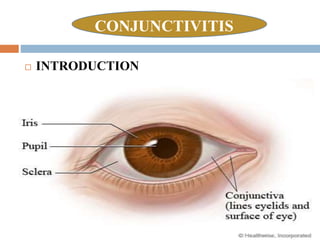
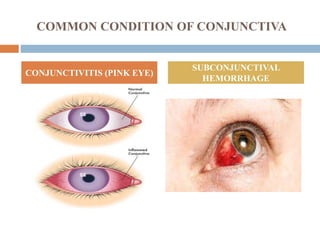
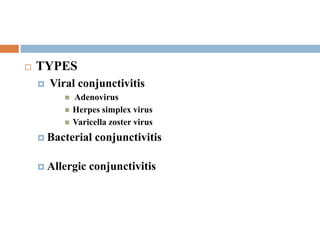
This document discusses three common eye disorders: cataracts, glaucoma, and conjunctivitis. It defines each disorder and describes their causes, risk factors, signs and symptoms, diagnostic tests, and treatment options. Cataracts involve cloudiness of the lens, glaucoma damages the optic nerve leading to vision loss, and conjunctivitis is an inflammation of the conjunctiva commonly known as pink eye. Surgical intervention may be required for cataracts and glaucoma to prevent further vision impairment.