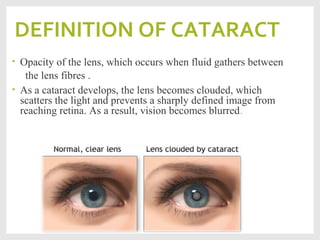
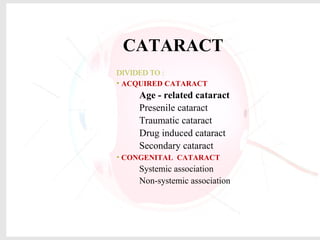
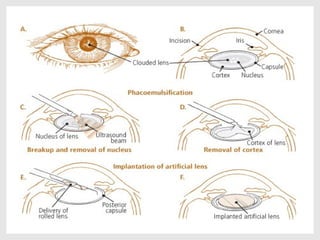
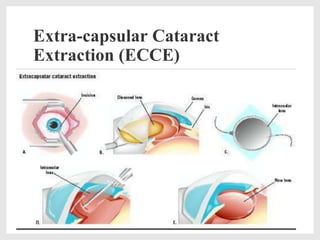
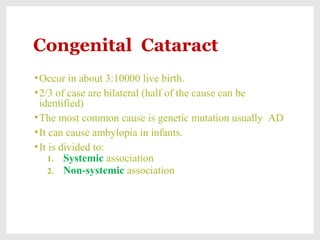
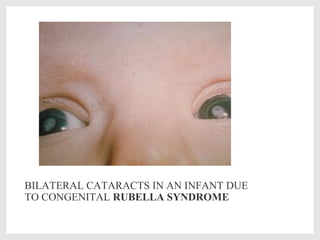
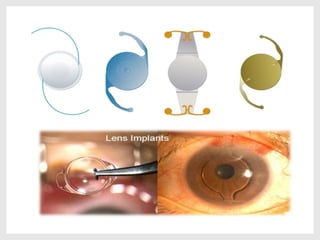
Cataract is an opacity of the lens that causes blurred vision. It occurs when fluid gathers between lens fibers. The most common cause is old age. Other causes include diseases like diabetes, previous eye surgeries, medications like steroids, trauma, radiation exposure, and congenital defects. Cataracts are classified as acquired or congenital and can be treated surgically by removing the opaque lens. Surgical techniques include phacoemulsification, extracapsular extraction, and intracapsular extraction. Postoperative care involves steroid and antibiotic eye drops to prevent complications.