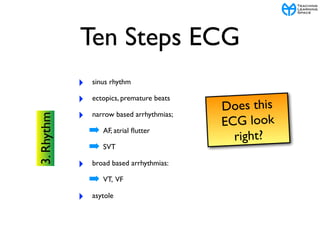
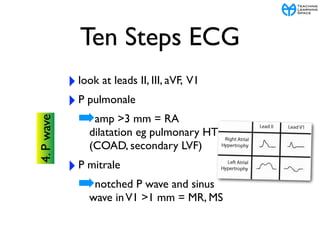
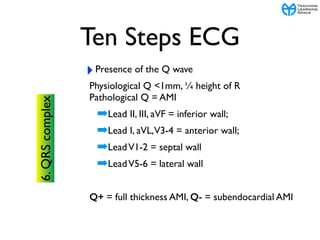
The document outlines the 10 step approach to interpreting electrocardiograms (ECGs) and presents two case studies from remote Aboriginal communities. It details the steps of an ECG including assessing the rate, rhythm, waves, intervals, segments, and complexes. The first case involves a 10 year old girl named Thomasina presenting with jerky movements and fever, who is diagnosed with rheumatic fever based on her ECG and blood tests. The second case describes a pilot named Frank who develops palpitations and is found to be in supraventricular tachycardia based on his ECG, which is terminated with carotid sinus massage.