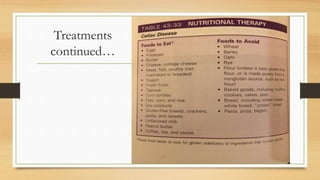
Johnny, an 8-year-old boy, is experiencing weight loss, abdominal discomfort, and loose stool. He has a history of type 1 diabetes and possible thyroid issues. Given his symptoms and medical history, celiac disease is a top consideration. Tests would include a small intestine biopsy to check for villi damage and serologic tests for antibodies associated with celiac disease. Celiac disease is an autoimmune response triggered by gluten that causes chronic inflammation and damages the small intestine. It is treated by maintaining a strict gluten-free diet.