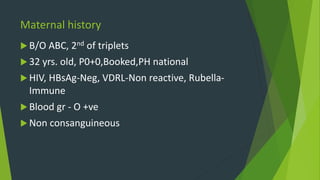
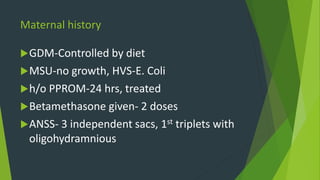
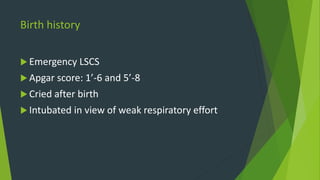
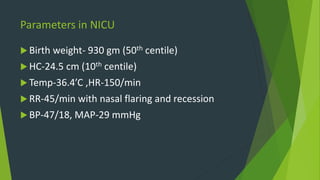
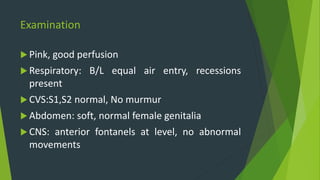
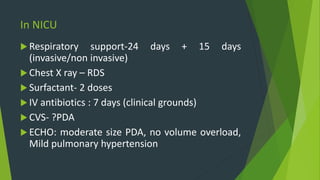
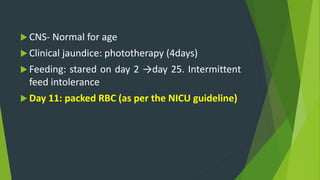
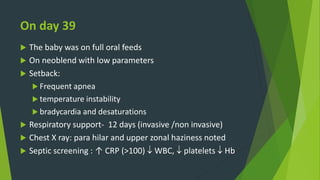
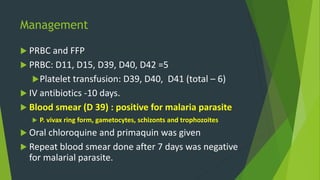
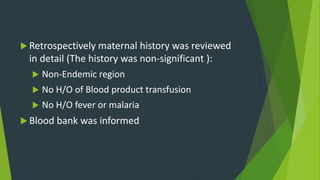
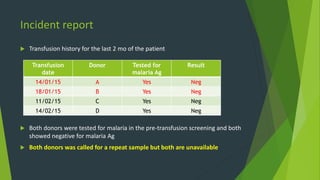
This document describes the case of a preterm infant born to a 32-year-old mother who developed malaria after receiving multiple blood transfusions in the NICU. The infant was born via emergency C-section at 32 weeks gestation. After an initial period of respiratory support, the infant developed fever, apnea, and declining vital signs. Blood tests showed anemia and elevated inflammatory markers. A blood smear revealed malaria parasites, and the infant was treated with antimalarial medications. The blood bank was notified, as the malaria was believed to have come from one of the five blood transfusions the infant received. Both donors tested negatively for malaria at the time of donation but could not be reached for retesting. The