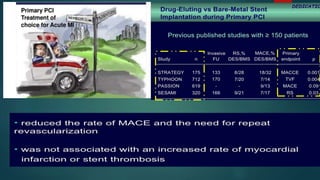
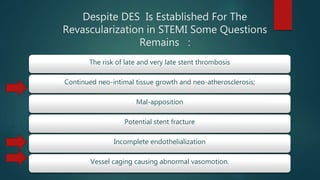
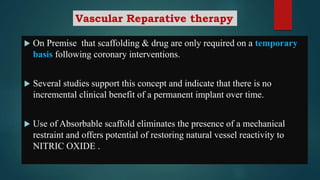
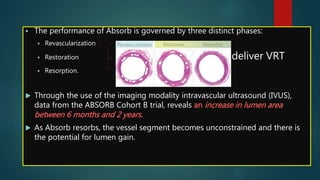
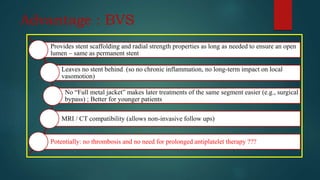
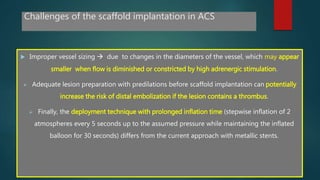
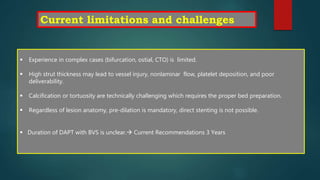
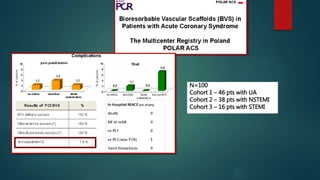
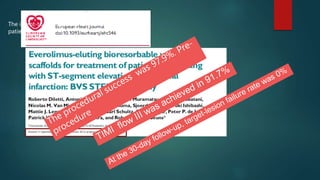
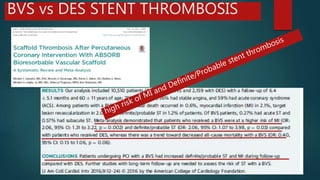
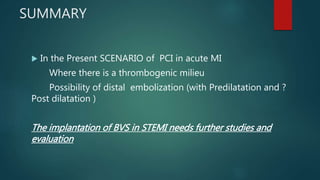
The document discusses the use of bioresorbable vascular scaffolds (BVS) in patients with ST-segment elevation myocardial infarction (STEMI). It summarizes that while BVS have shown efficacy and safety in trials so far, their use in STEMI patients remains uncertain due to challenges such as improper vessel sizing in acute settings, risk of distal embolization, and limited data on dual antiplatelet therapy duration. More studies are needed to fully evaluate the risks and benefits of deploying BVS in patients with acute MI.