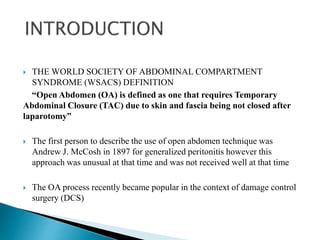
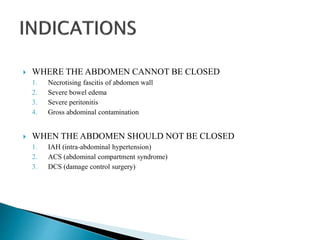
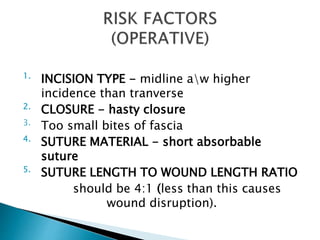
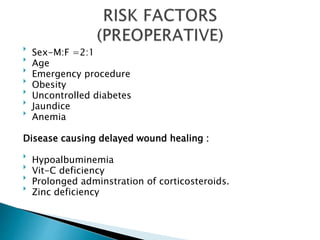
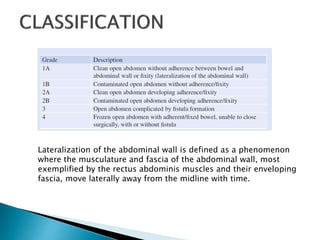
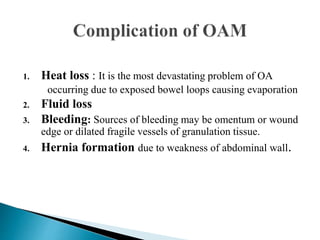
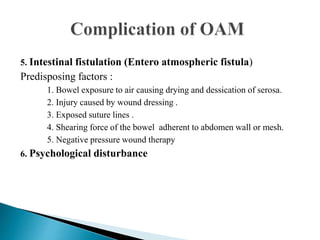
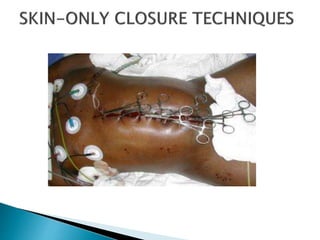
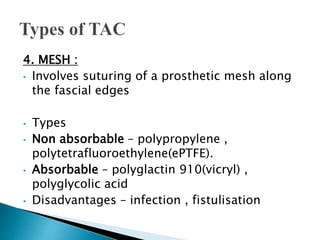
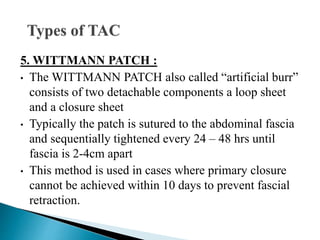
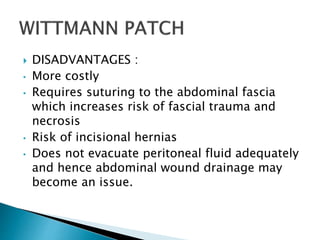
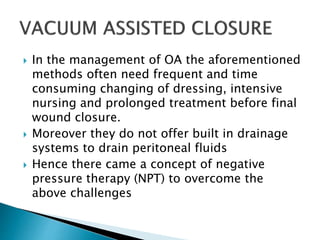
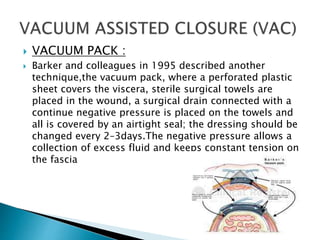
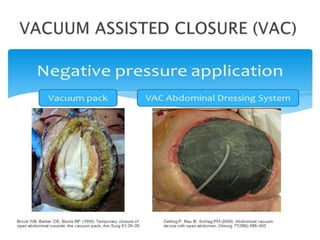
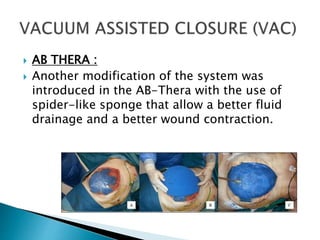
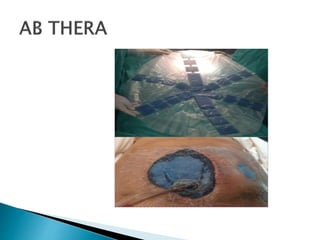
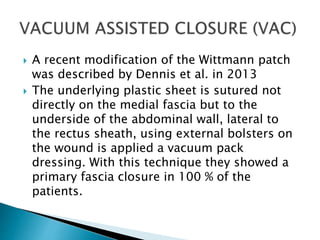
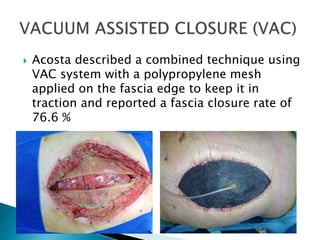
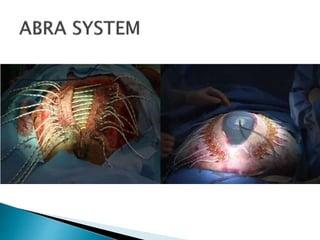
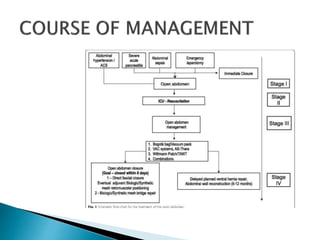
The document discusses open abdomen techniques and management. It defines open abdomen as requiring temporary abdominal closure after laparotomy when the skin and fascia cannot be primarily closed. Common causes for open abdomen include necrotizing fasciitis, severe bowel edema, peritonitis, and gross abdominal contamination. Temporary abdominal closure techniques discussed include simple packing, skin closure, Bogota bag, mesh, and Wittmann patch. More recently, negative pressure wound therapy including vacuum-assisted closure and variants like AB Thera have gained popularity due to advantages like improved drainage and wound contraction allowing higher rates of fascial reapproximation. The main goal of open abdomen treatment remains achieving definitive abdominal wall closure, preferably within 8 days to reduce complications.