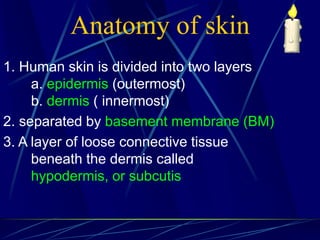
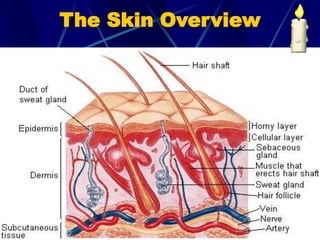
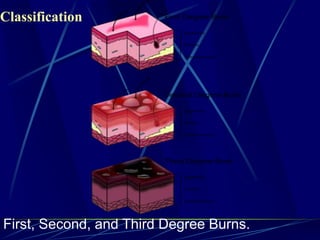
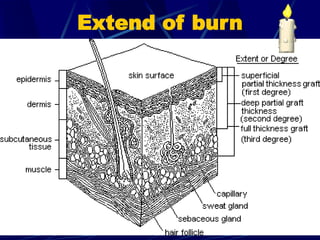
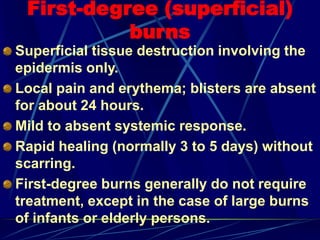
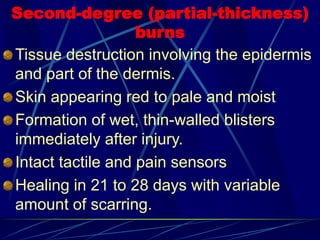
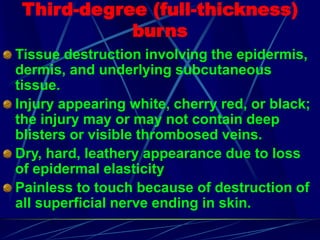
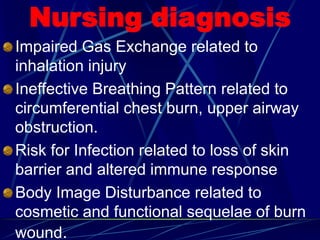
Burns are skin injuries caused by heat, flames, electricity, chemicals, friction, or sunlight. The severity depends on the depth of injury - first degree burns involve the outer layer of skin while third degree burns extend deeper. Proper burn care includes stopping the burning, removing clothing, ensuring an open airway, cooling the burn, treating for shock, preventing infection, managing pain, and addressing physical and emotional needs during recovery.