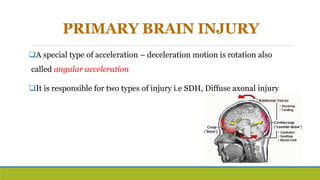
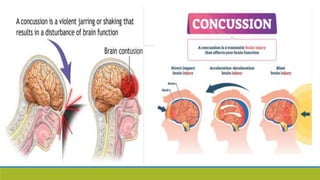
This document discusses cranio-cerebral injuries or traumatic brain injuries. It defines these injuries as damage to the skull or brain that interferes with normal function. It then discusses the classification, etiology, mechanisms of injury, diagnosis and management of such injuries. Traumatic brain injuries can be classified based on severity using the Glasgow Coma Scale or based on location of the injury in the brain. The mechanisms of injury include both primary injuries caused directly by the trauma and secondary injuries caused by processes initiated after the trauma such as increased intracranial pressure. Diagnosis involves tests such as CT scans and management focuses on stabilization, monitoring, controlling increased intracranial pressure and addressing complications.