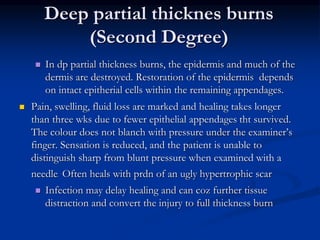
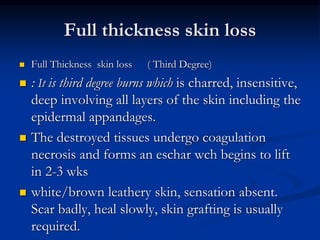
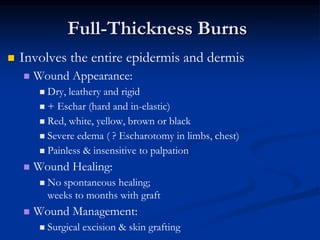
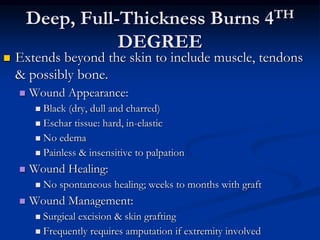
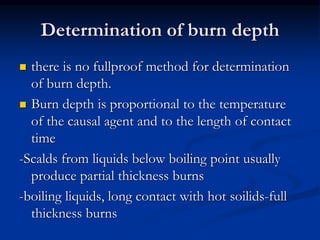
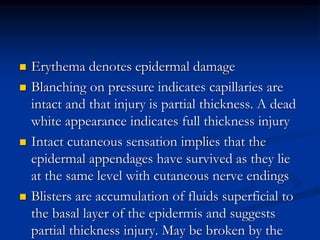
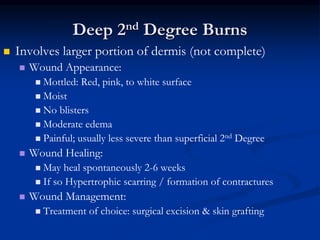
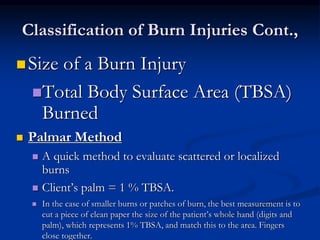
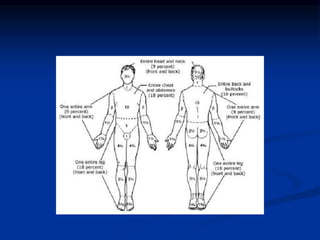
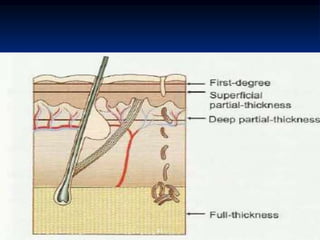
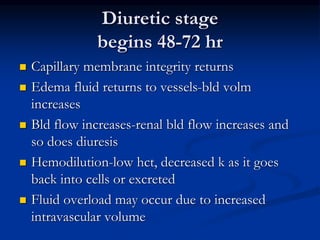
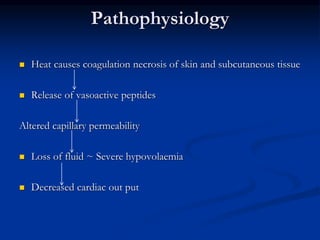
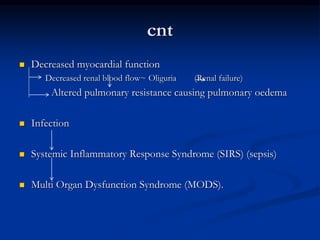
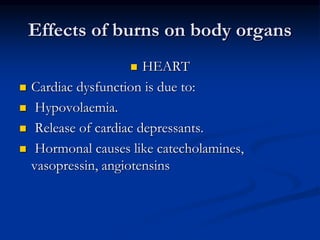
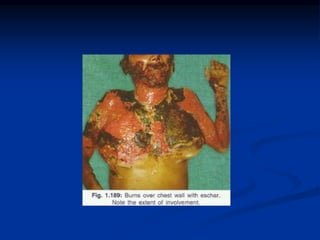
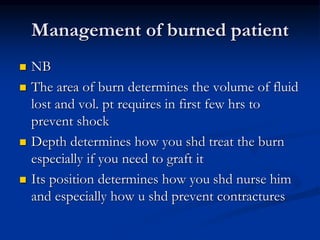
Burns are injuries to tissues caused by heat, friction, electricity, radiation or chemicals. They can damage the skin, airways, lungs, circulation, gut and immune system. The severity is classified by depth and size of the burned area. First degree burns only affect the outer layer of skin while fourth degree burns extend deeper to involve muscles and bones. Proper assessment of burn depth and size is important for treatment. Burns increase inflammation and alter blood vessel permeability, causing fluid shifts that can cause shock. They also impair the immune system, increasing risk of infection.