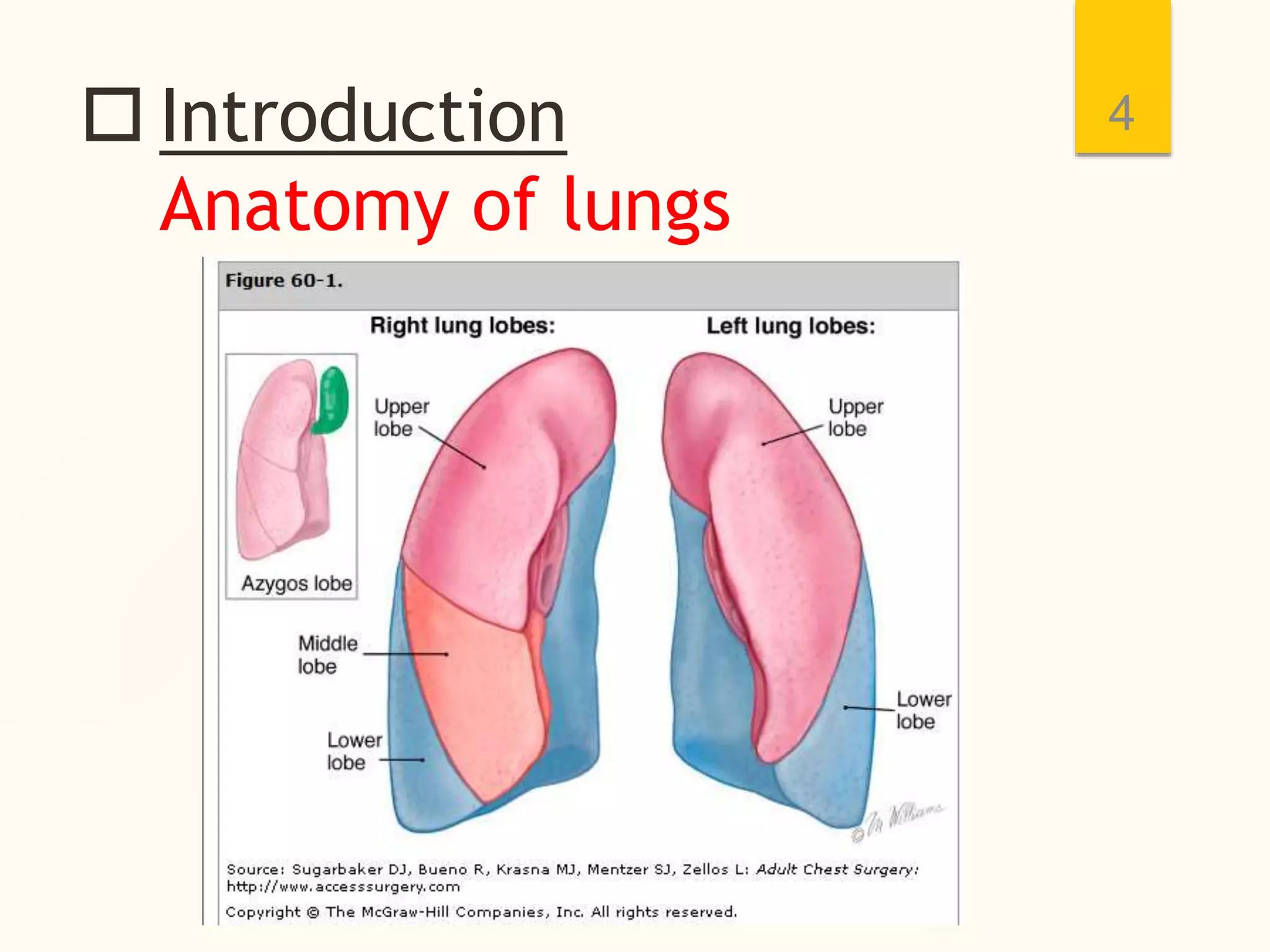
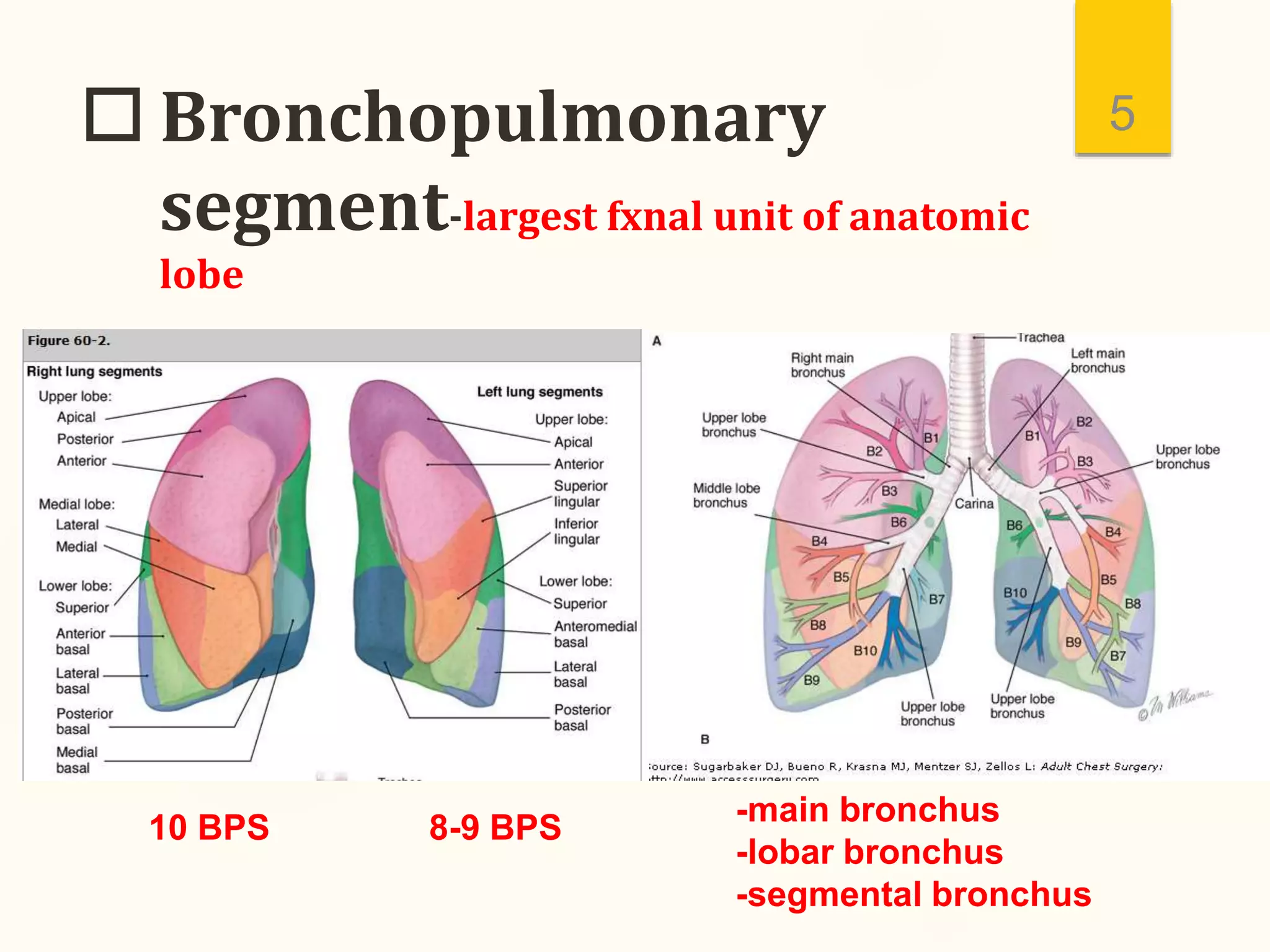
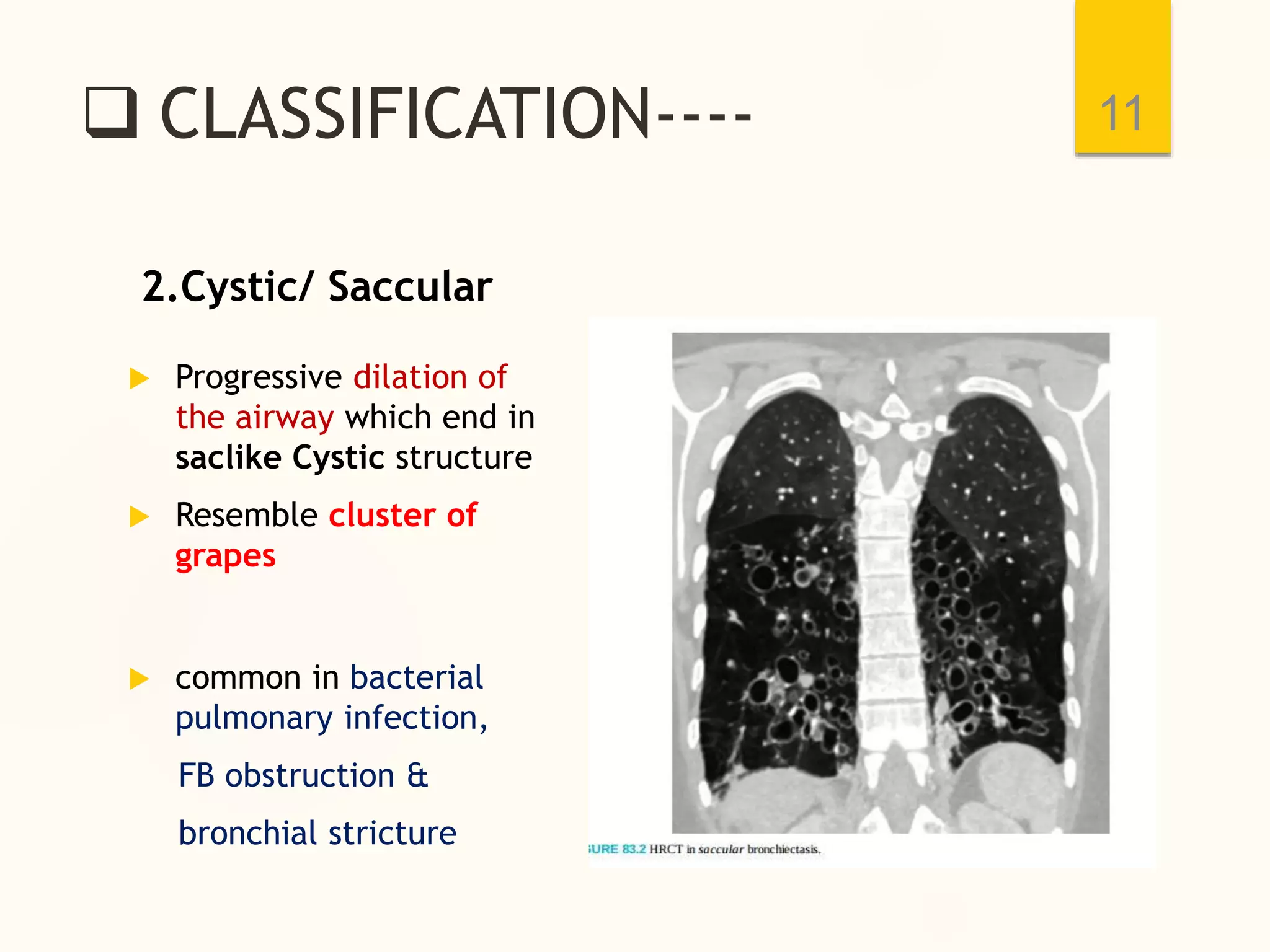
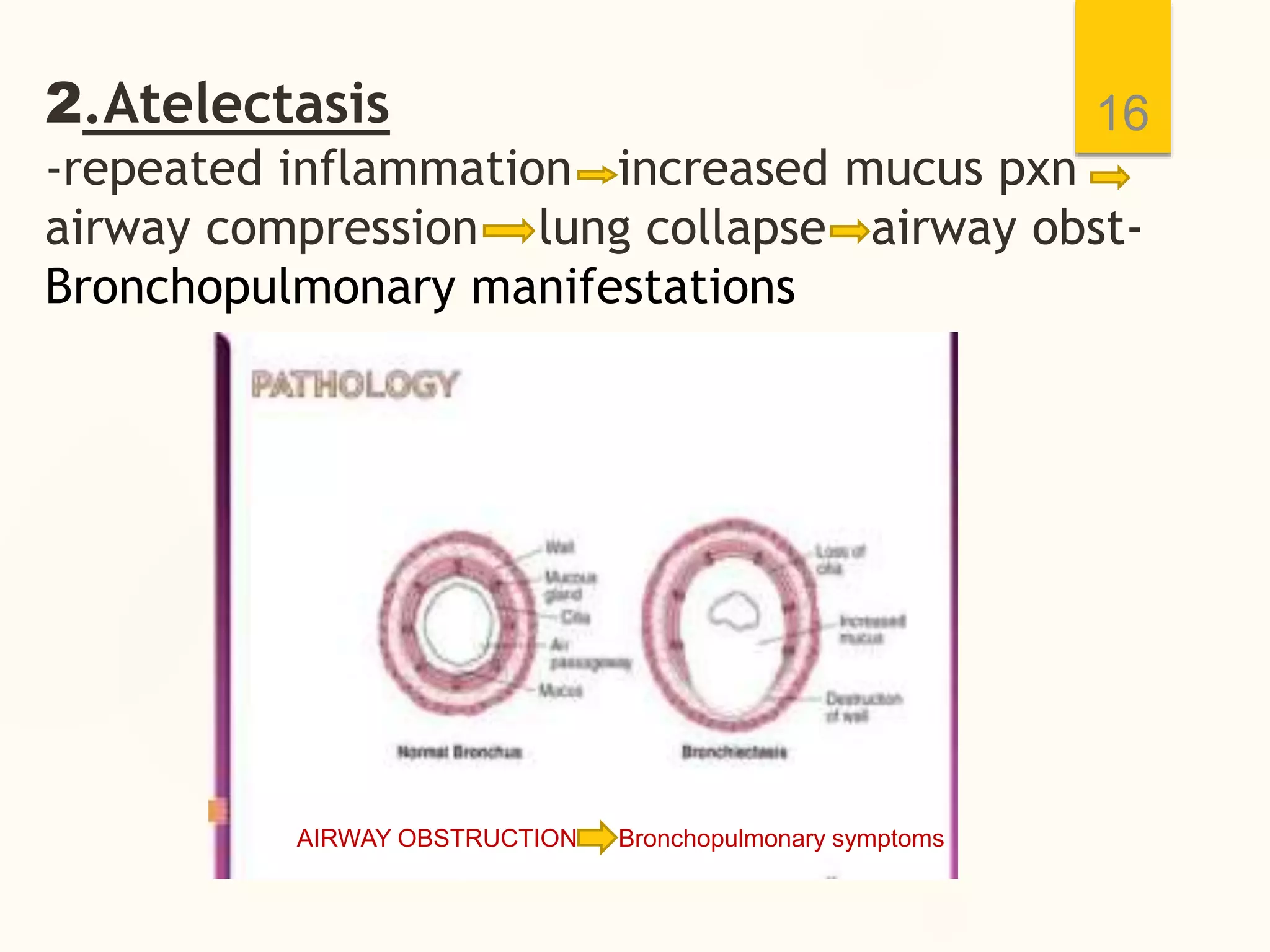
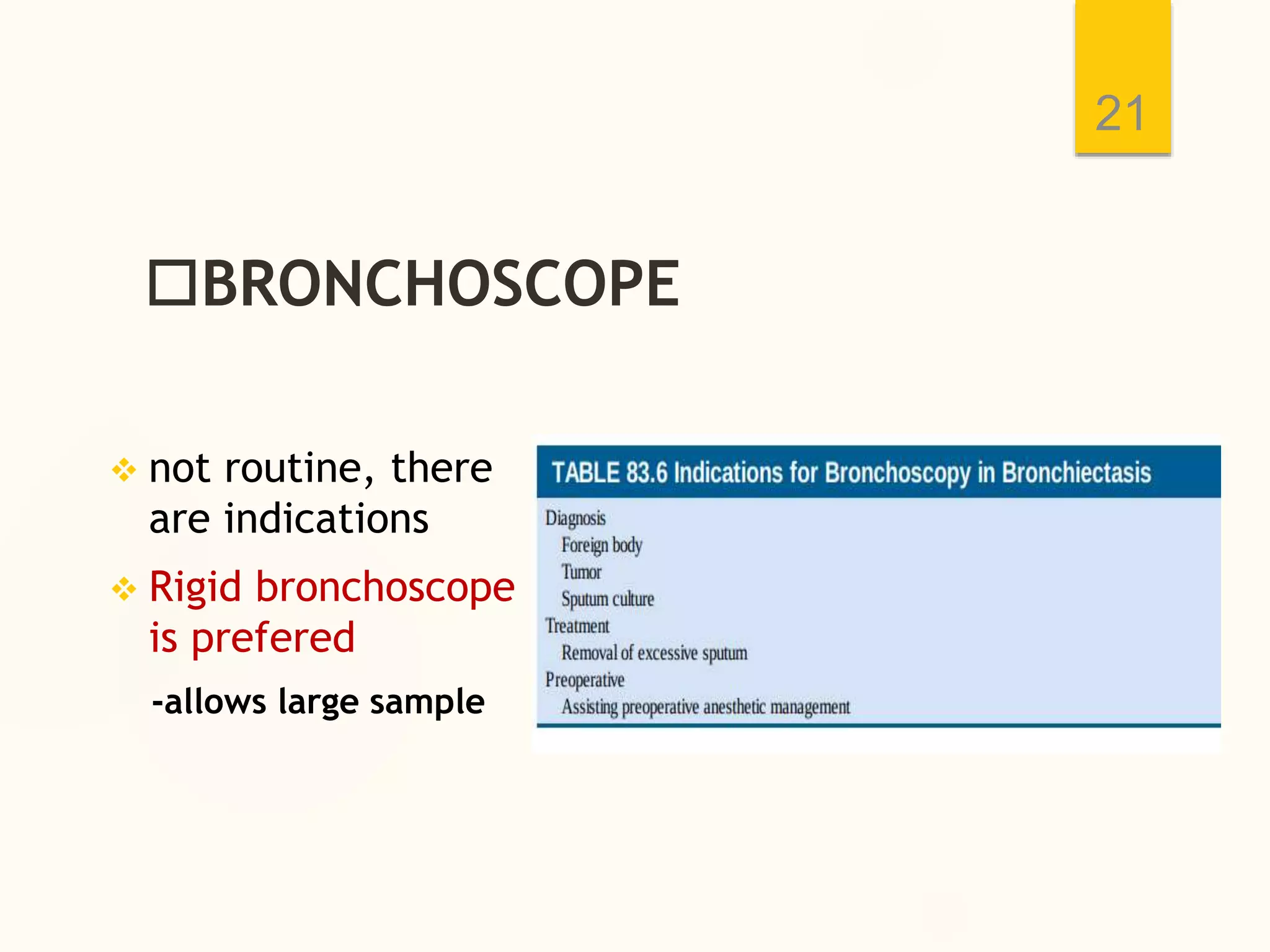
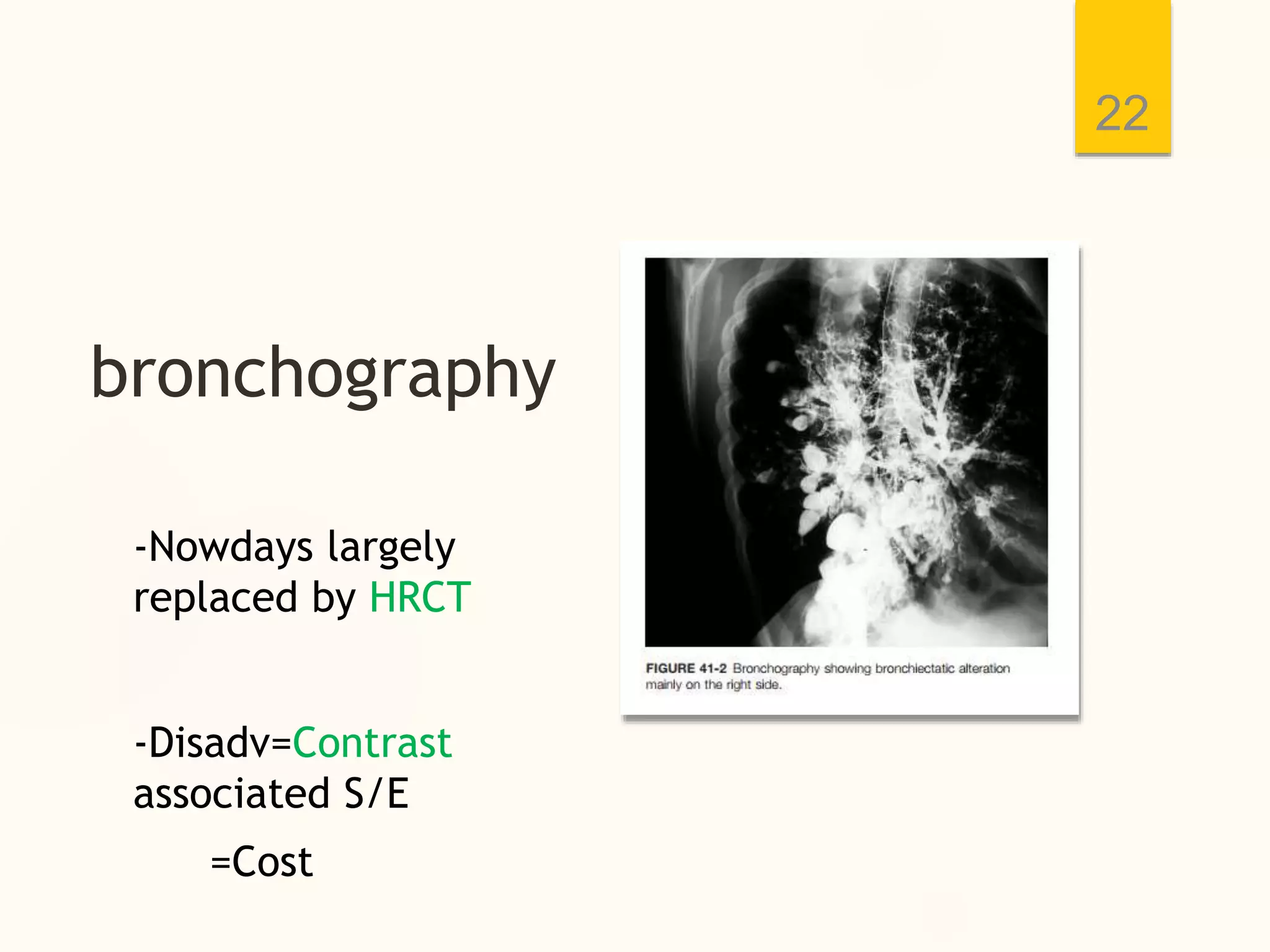
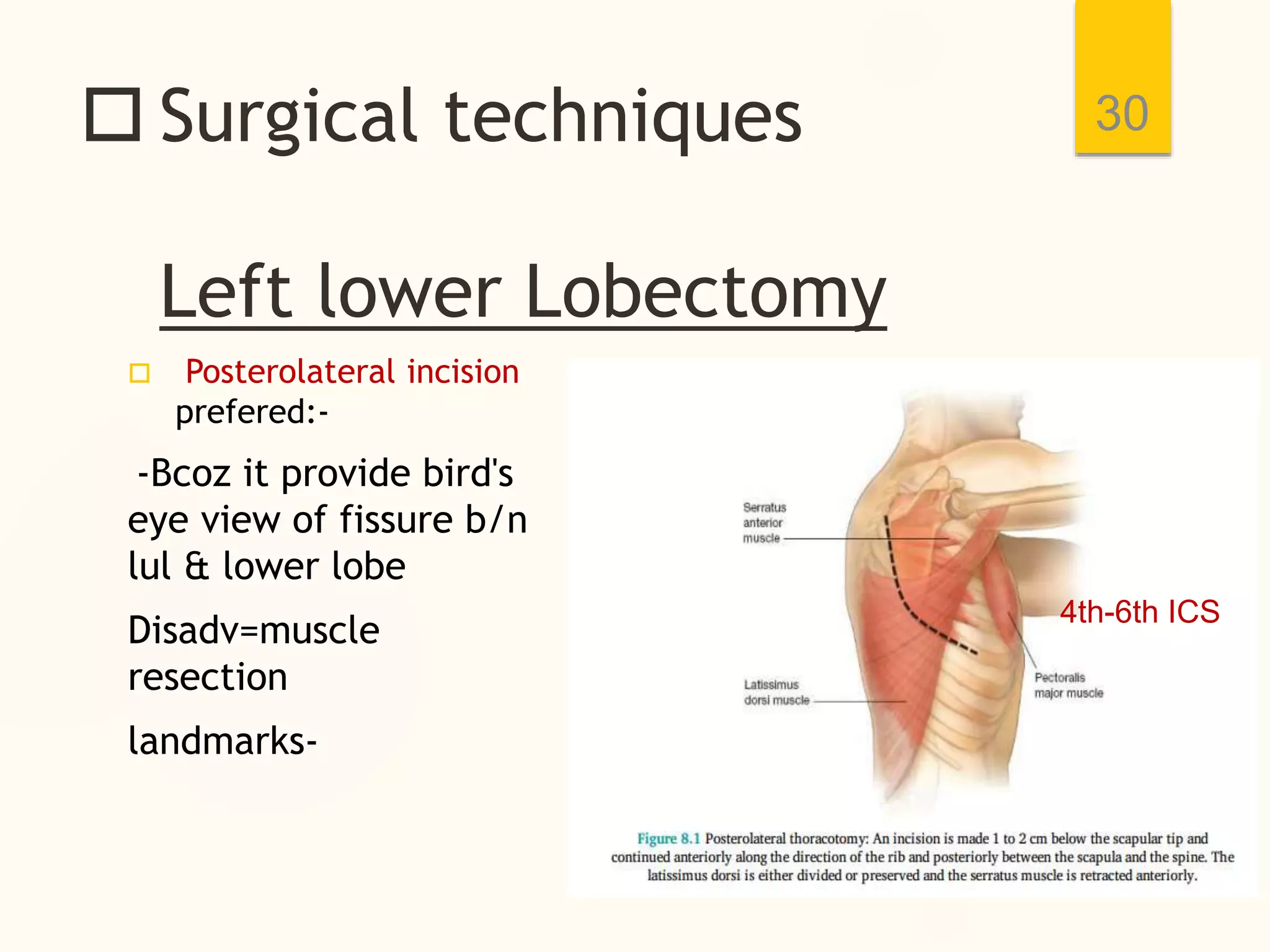
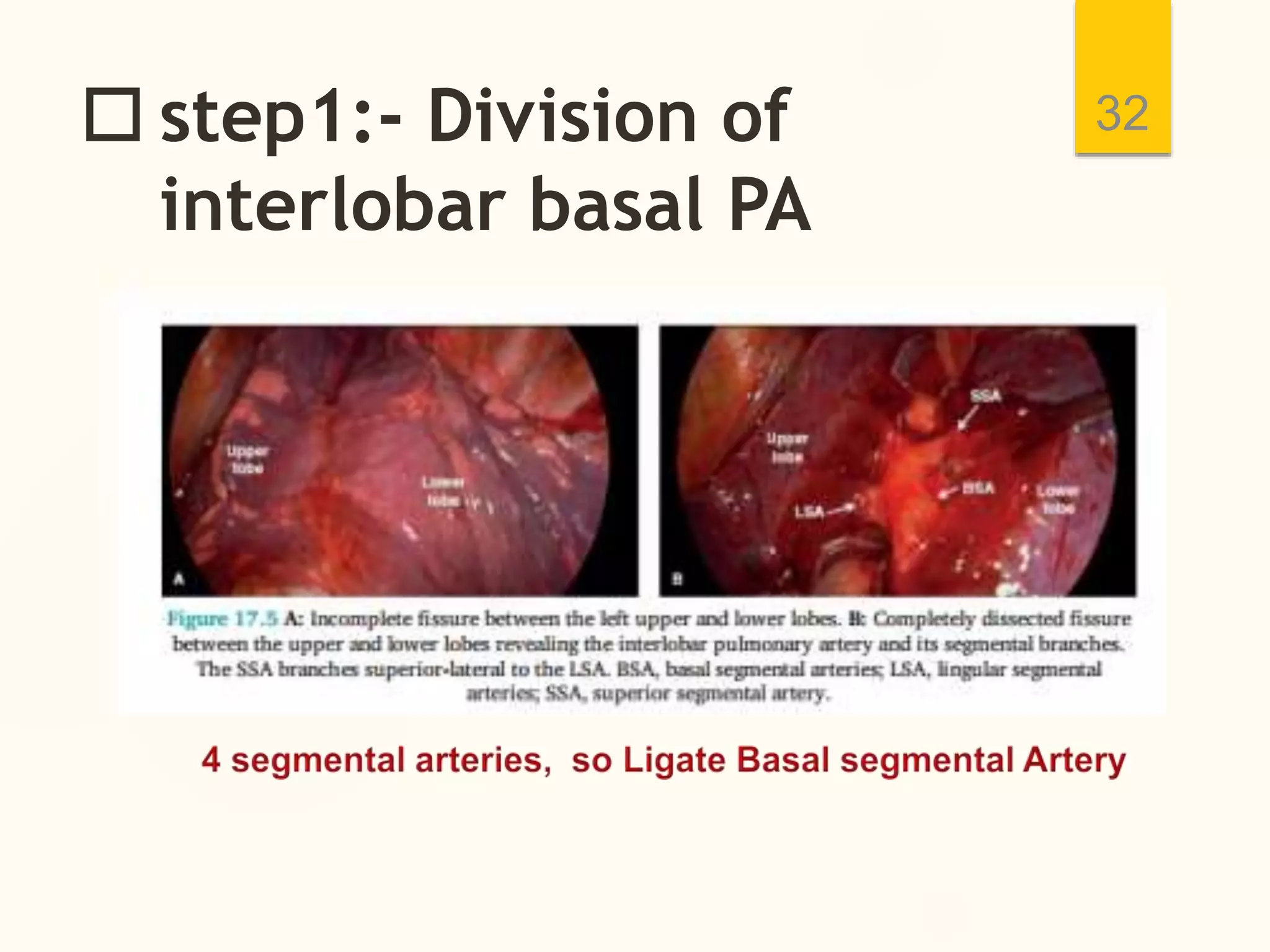
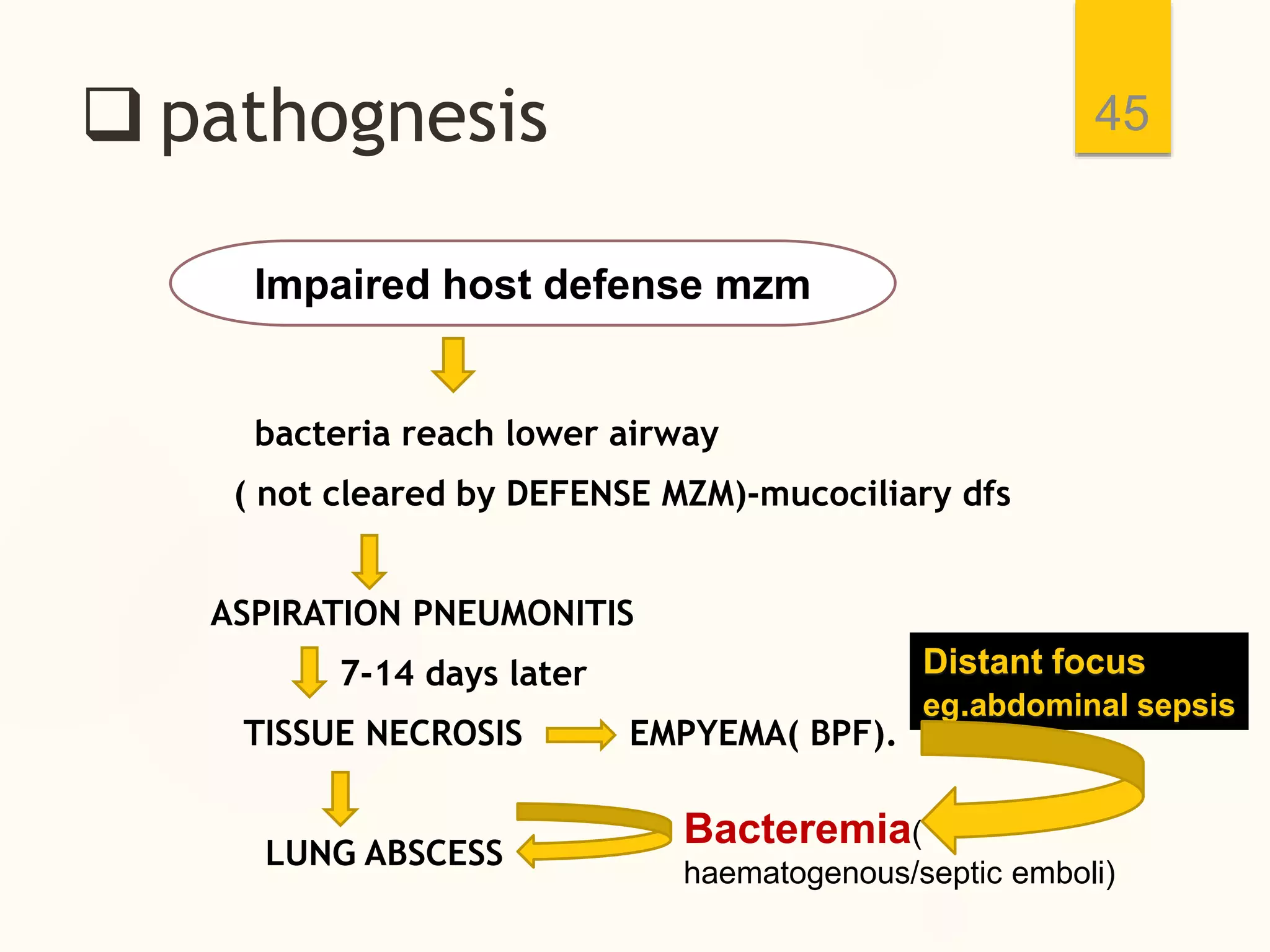
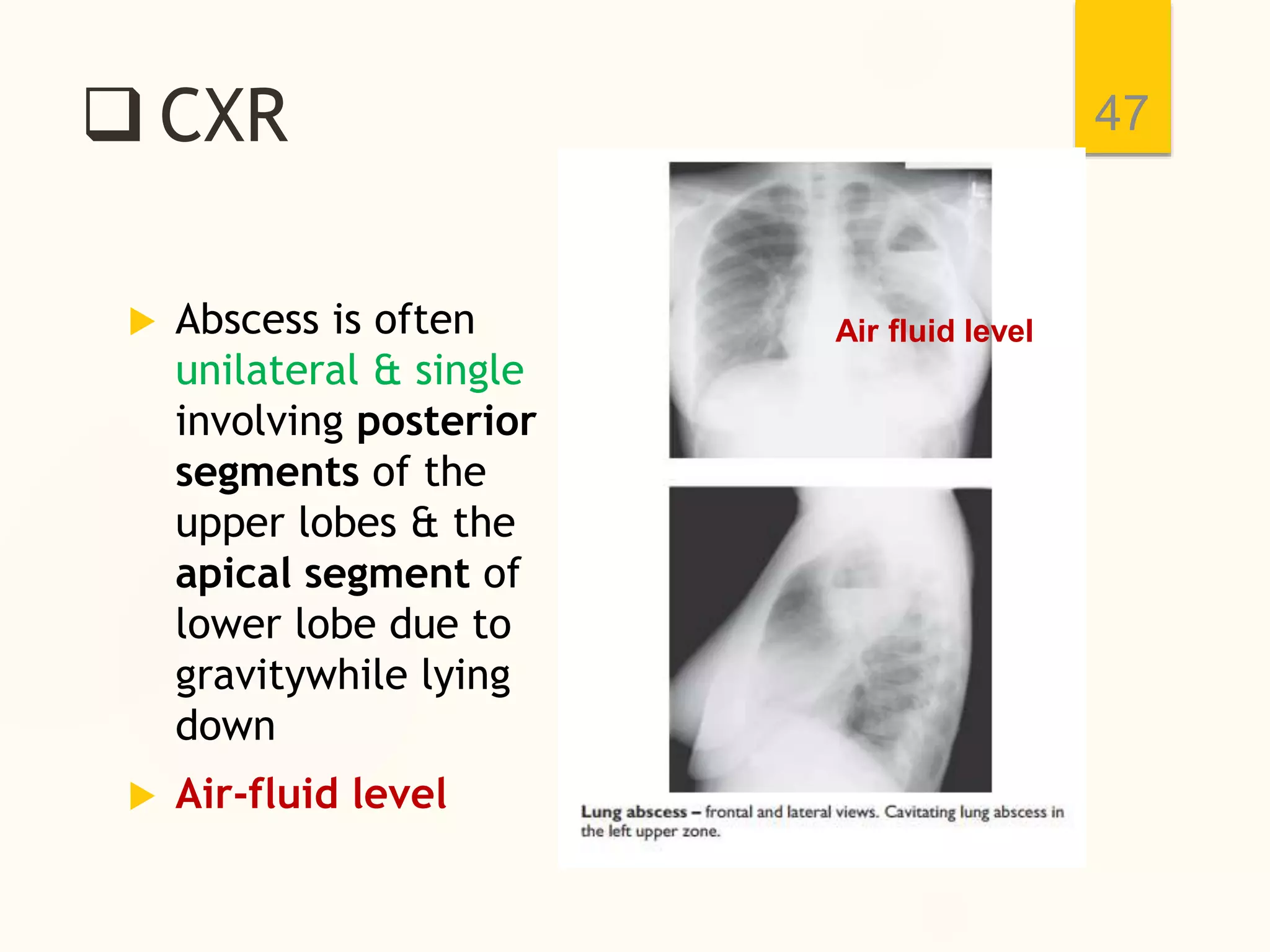
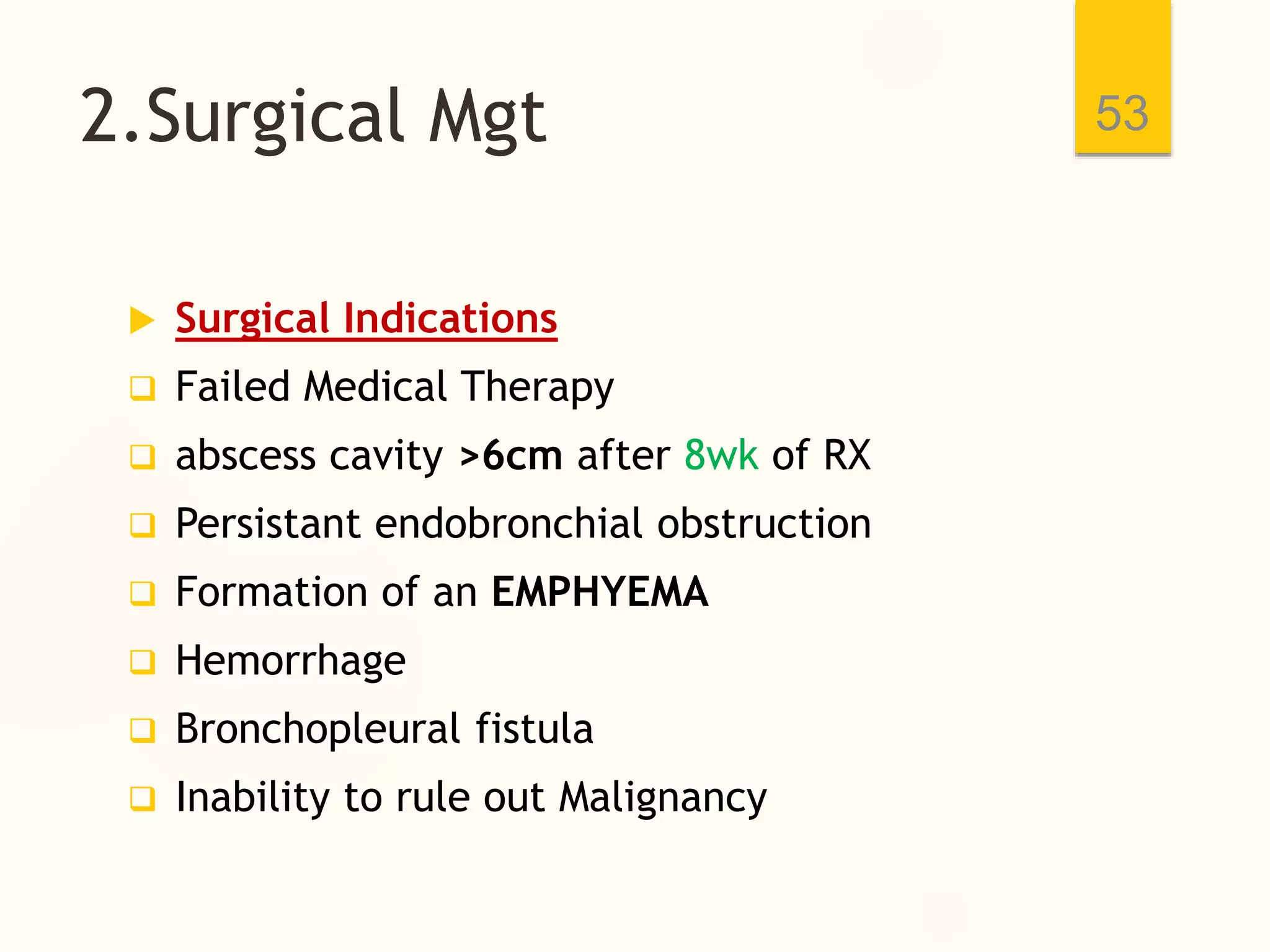
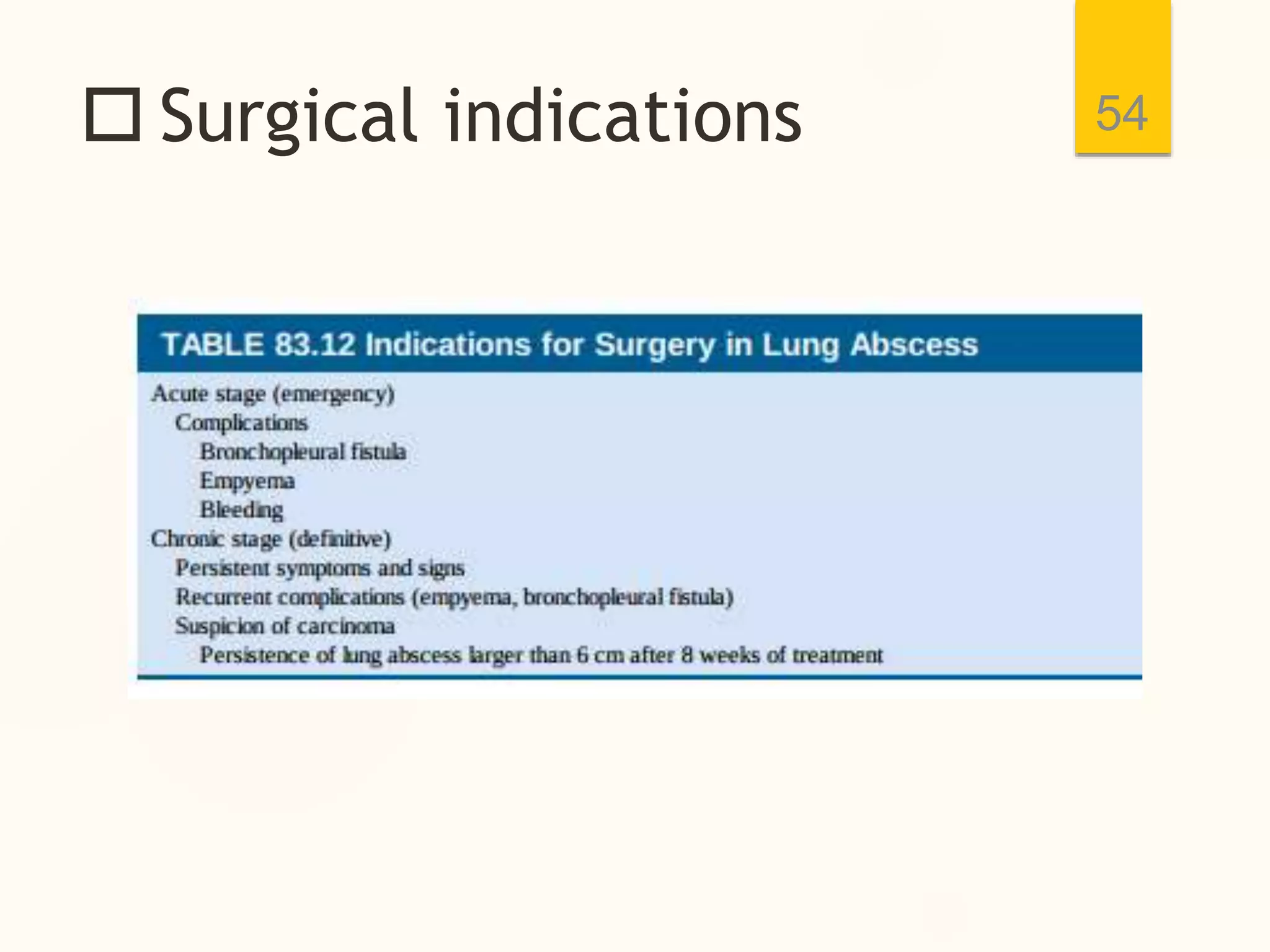
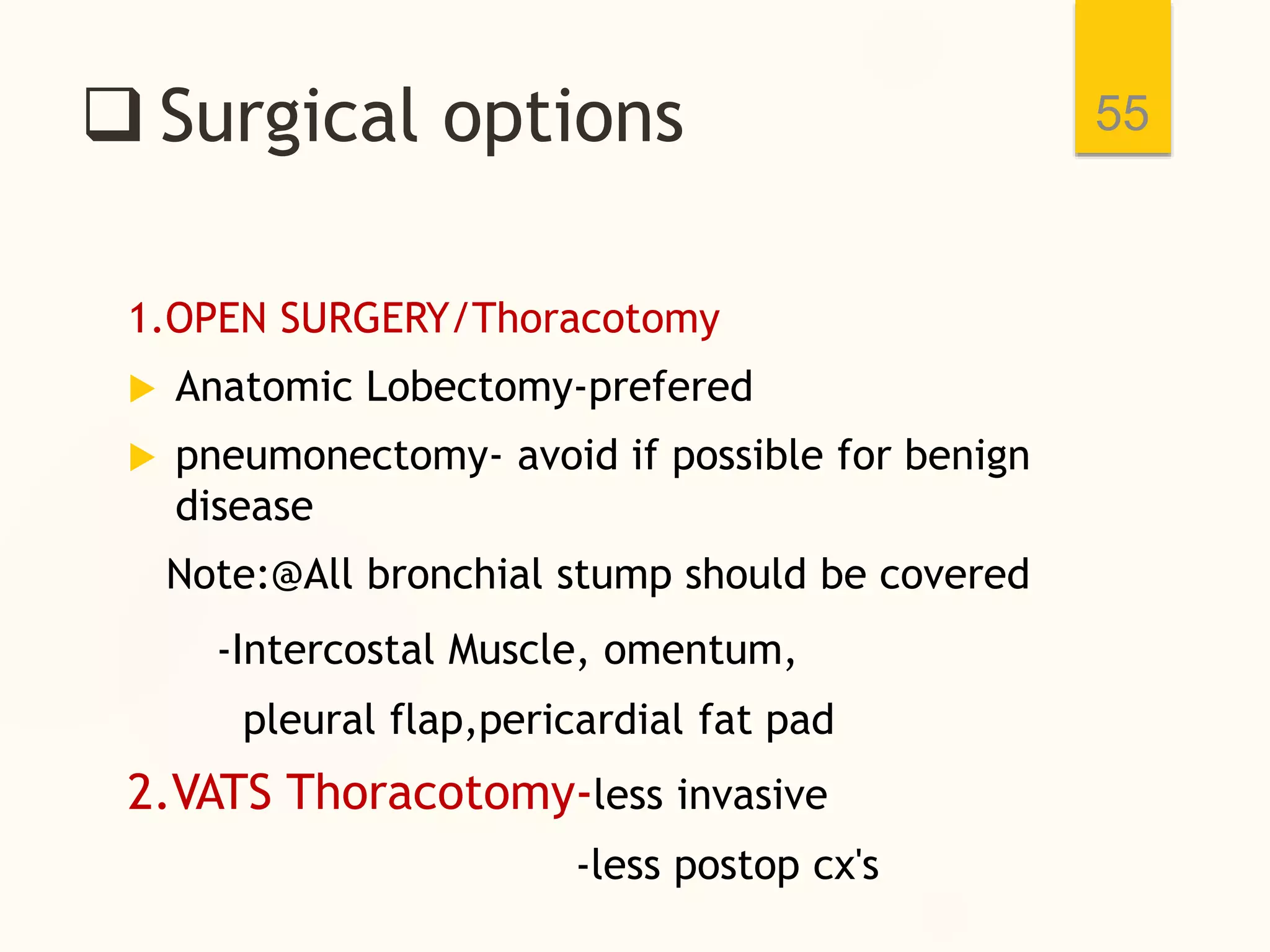
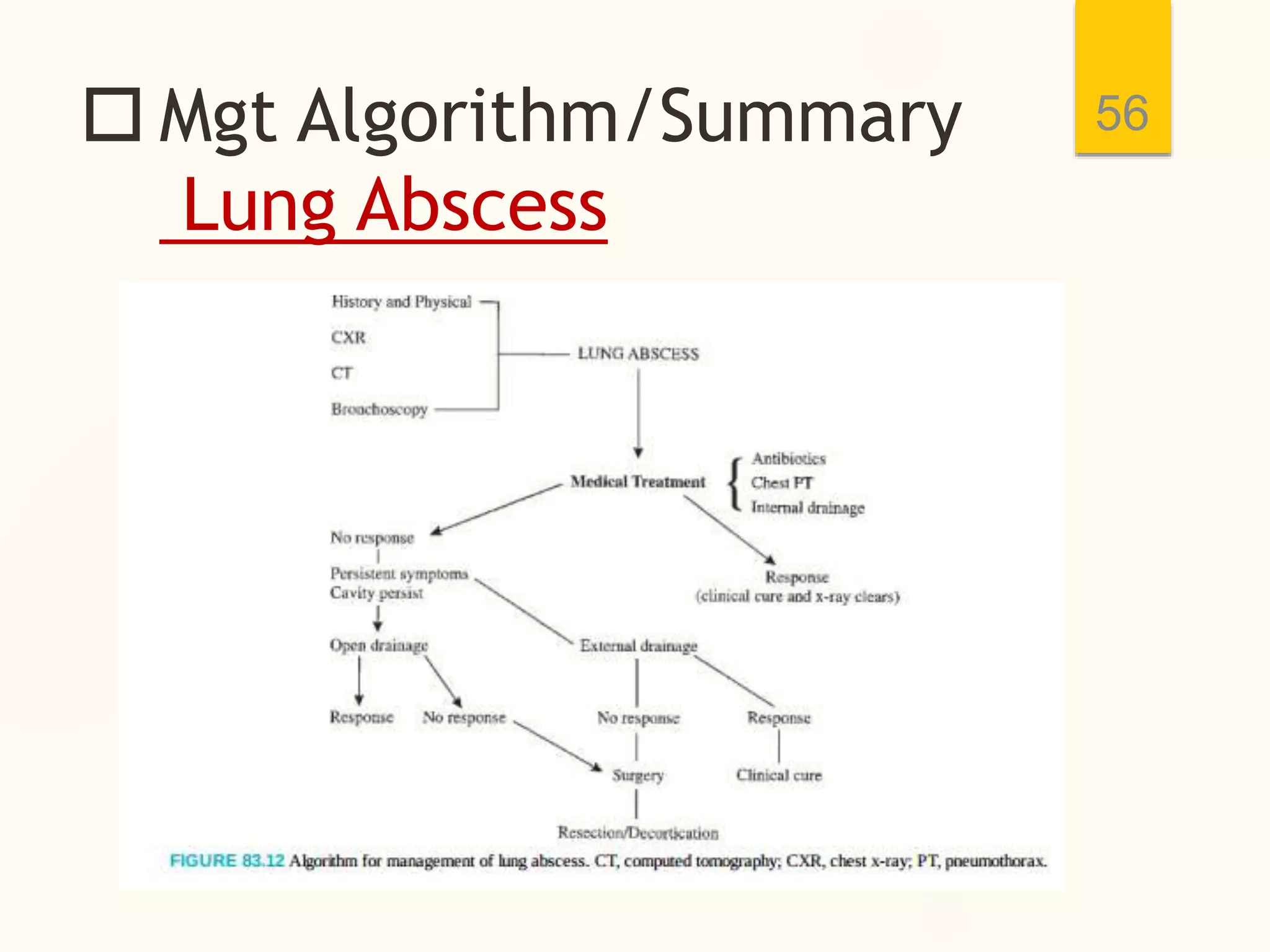
The document discusses the management of suppurative lung diseases, specifically bronchiectasis and lung abscess, highlighting their definitions, etiologies, clinical features, and treatment options. It covers various management strategies including medical interventions, surgical options, and diagnostic imaging methods for effective disease management. The document emphasizes the importance of a multidisciplinary approach and outlines prognostic factors associated with these lung conditions.