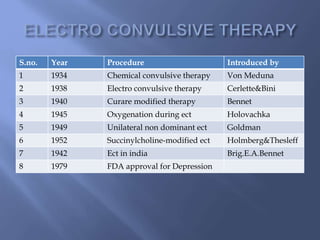
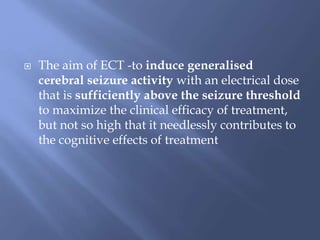
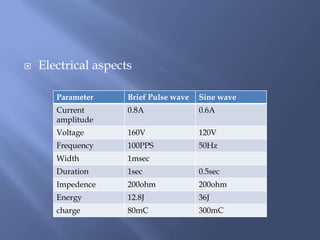
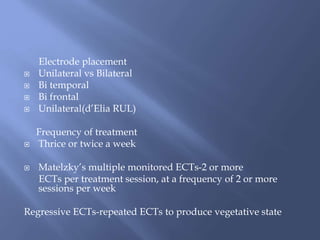
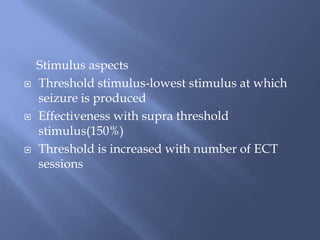
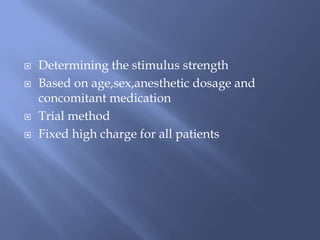
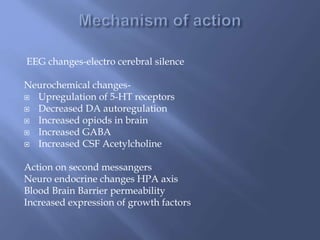
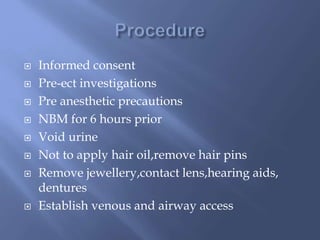
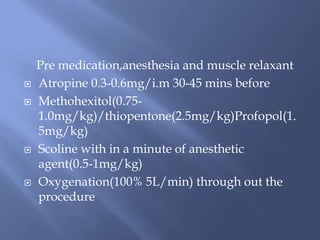
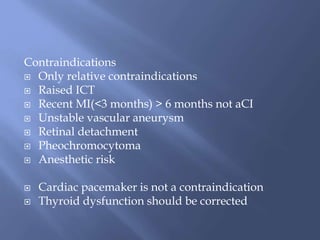
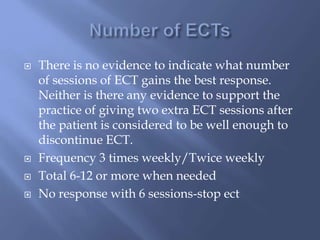
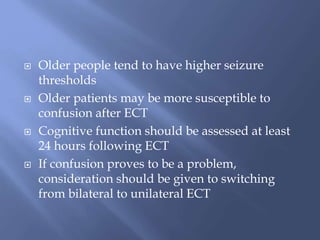
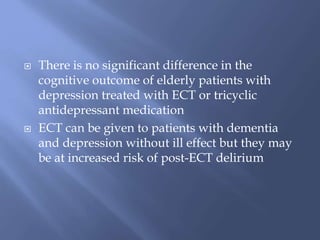
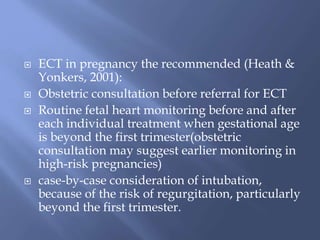
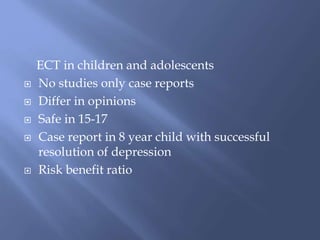
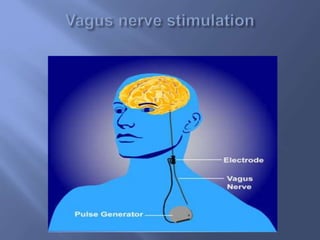
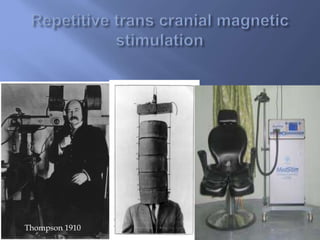
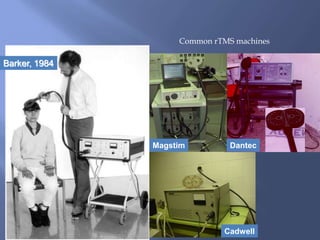
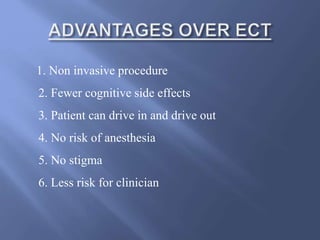
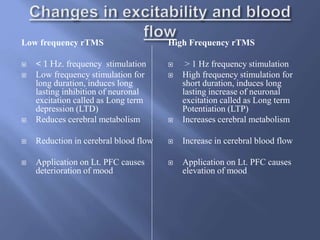
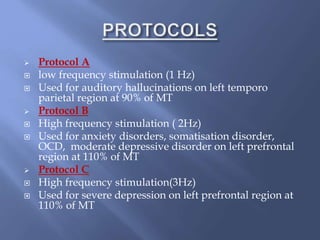
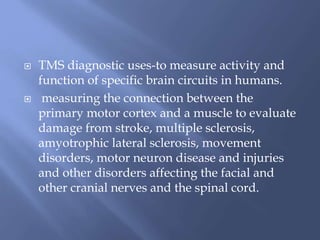
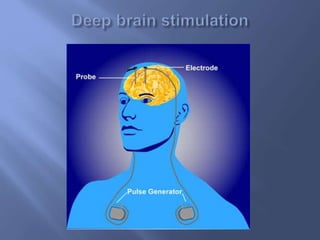
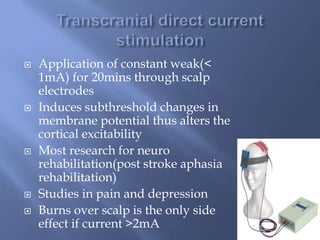
This document provides information on various brain stimulation therapies, including electroconvulsive therapy (ECT), vagus nerve stimulation (VNS), transcranial magnetic stimulation (TMS), and deep brain stimulation (DBS). It discusses the history, procedures, indications, side effects, and mechanisms of action for each therapy. ECT involves inducing seizures with electricity to treat conditions like depression. VNS uses electrical pulses to the vagus nerve to treat epilepsy and depression. TMS uses magnetic pulses to target specific brain regions without surgery. These non-pharmacological therapies can be effective options for treating neuropsychiatric illnesses.