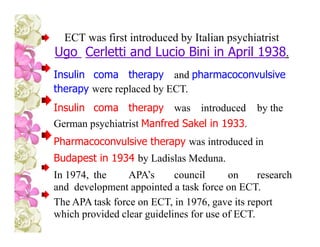
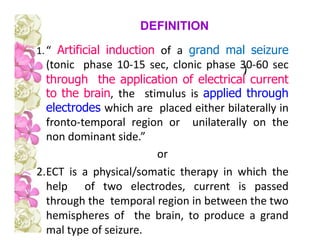
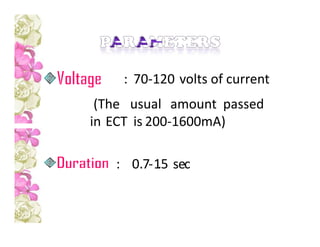
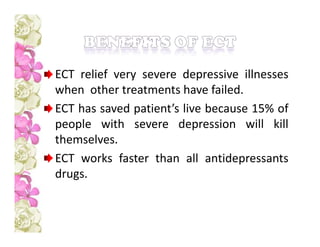
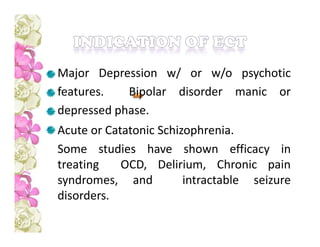
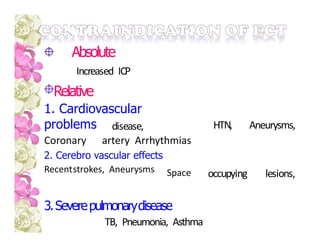
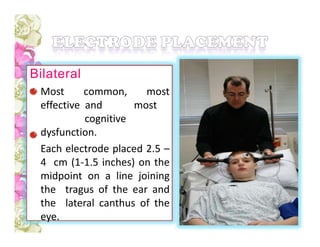
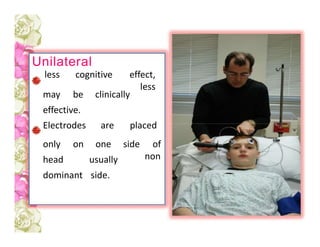
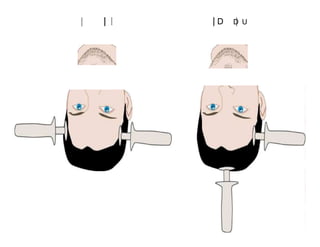
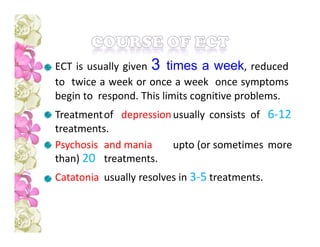
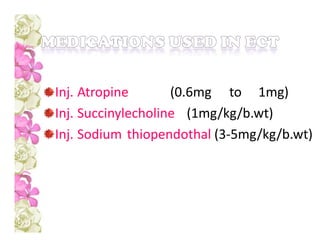
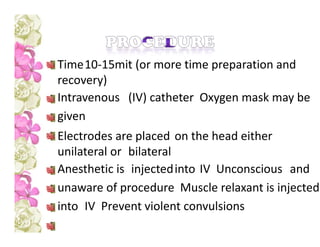
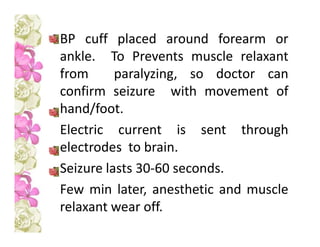
ECT involves inducing seizures through electrical stimulation of the brain under anesthesia to treat psychiatric conditions. It was introduced in 1938 and replaced previous somatic therapies. ECT works via its effects on brain catecholamine pathways and limbic systems. The procedure involves placing electrodes on the head and passing a brief electrical current while the patient is under anesthesia and muscle relaxation to induce a seizure. Potential risks include cognitive side effects and medical complications, though memory loss is usually temporary. Informed consent is required but involuntary treatment is allowed under certain legal circumstances.