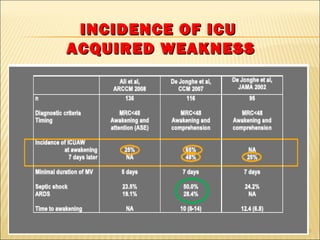
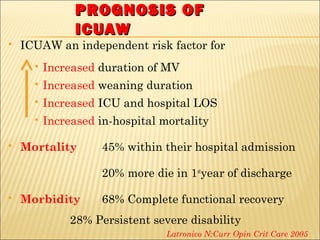
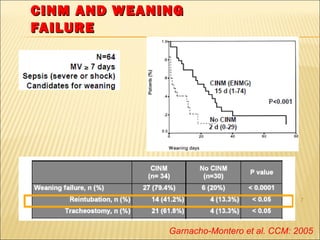
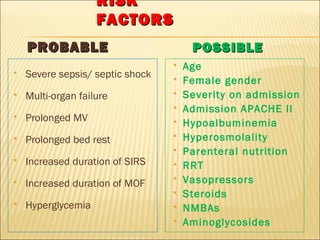
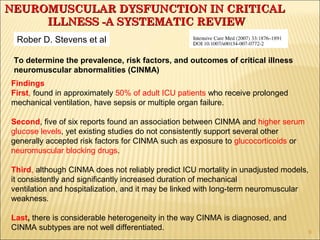
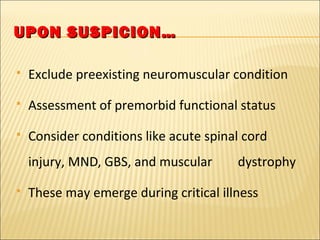
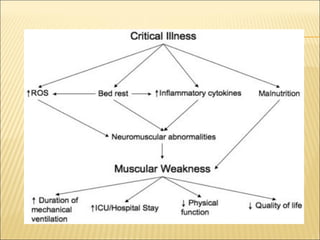
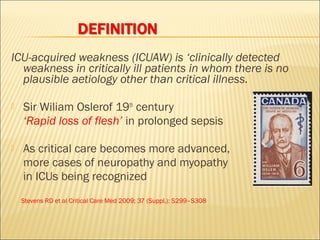
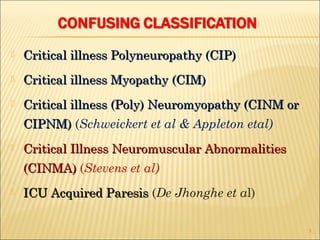
This document discusses critical illness-acquired weakness (ICUAW), including its prevalence, risk factors, outcomes, and diagnostic criteria. The main points are:
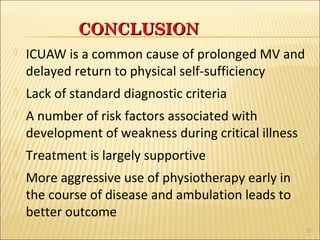
First, ICUAW occurs in approximately 50% of adult ICU patients receiving prolonged mechanical ventilation or those with sepsis/multiple organ failure.
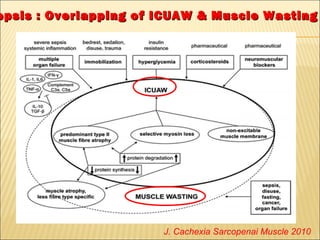
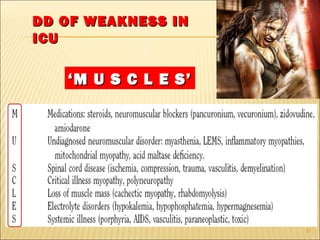
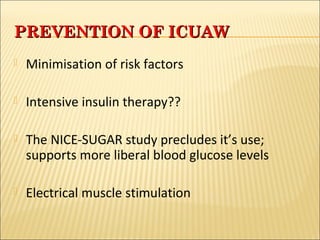
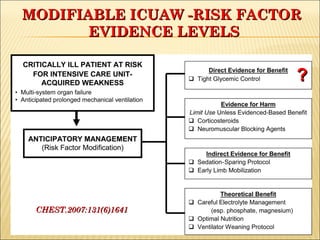
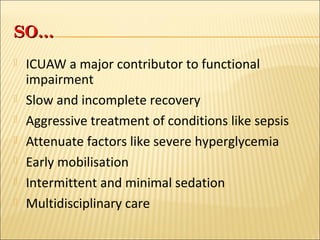
Second, while hyperglycemia is associated with ICUAW, studies have not consistently supported other accepted risk factors like glucocorticoids or neuromuscular blockers.
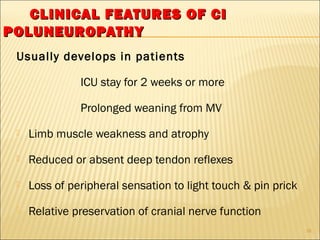
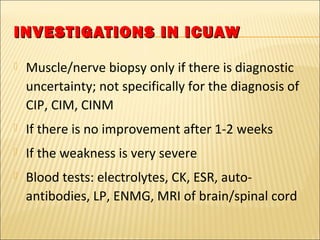
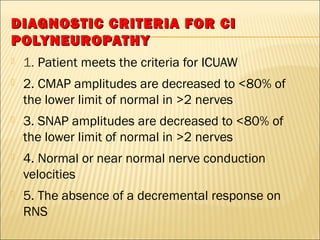
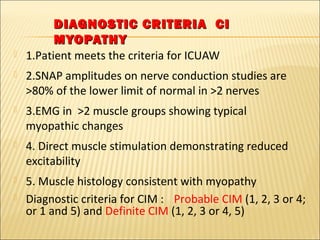
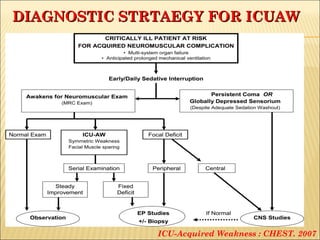
Third, ICUAW increases duration of mechanical ventilation and hospitalization, and may cause long-term neuromuscular weakness, though it does not reliably predict mortality. Diagnosis is challenging due to heterogeneity.
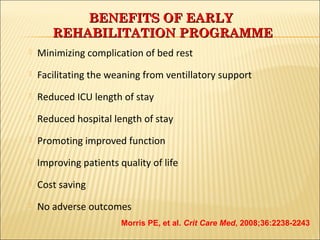
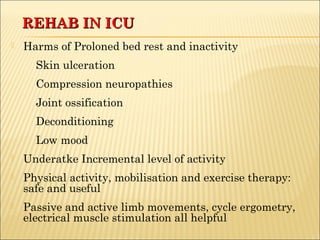
Early rehabilitation and mobil
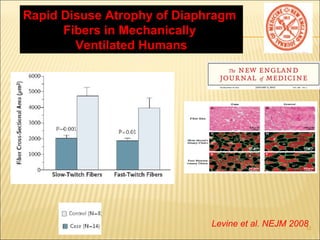
![ Prevalence of 46% [95% CI]
Prevalence of CIM
7% after OLTx
36% in status asthmaticus
35% COPD severe acute exacerbations
4](https://image.slidesharecdn.com/icuawmaster-140915114108-phpapp01/85/ICU-Acquired-Weakness-4-320.jpg)