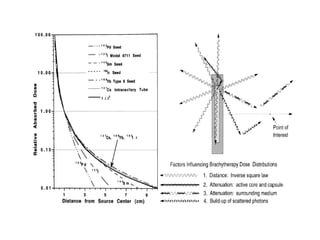
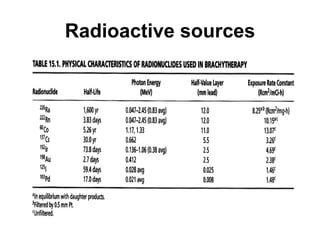
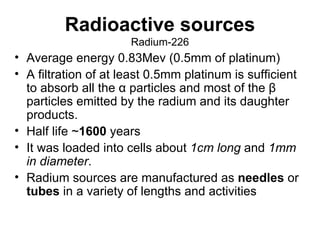
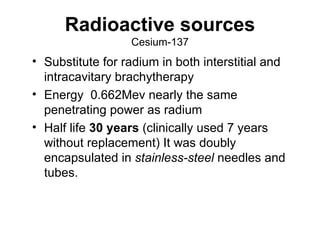
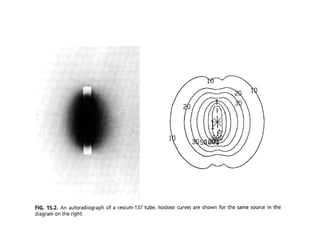
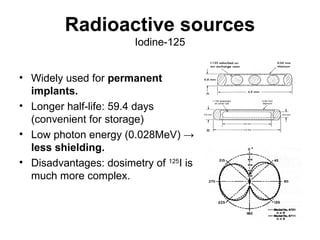
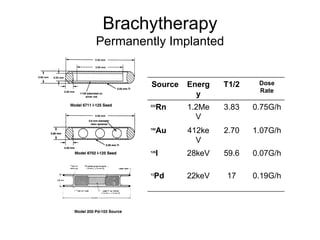
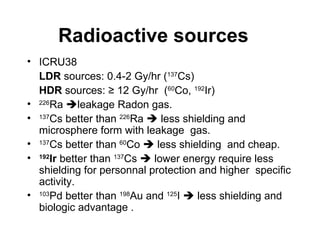
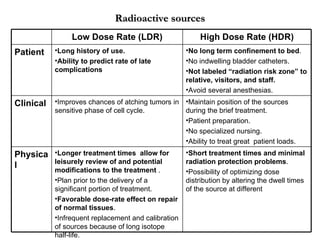
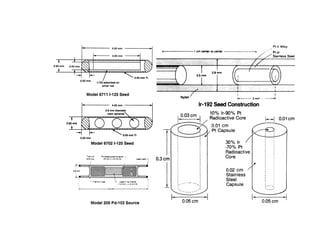
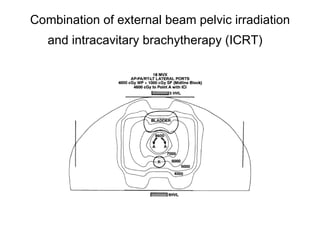
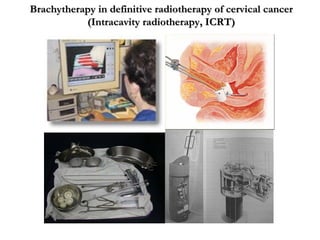
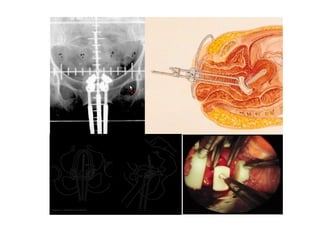
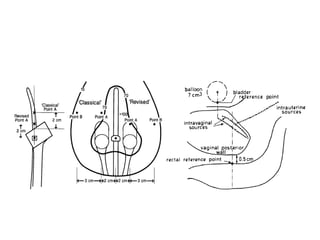
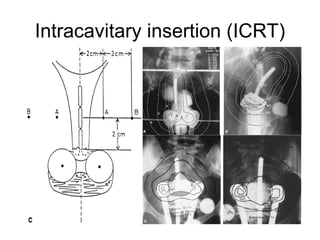
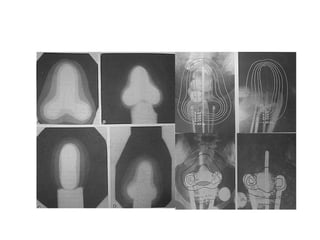
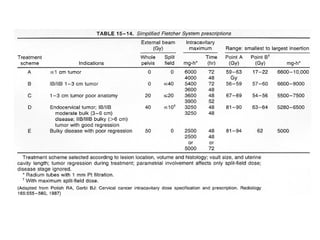
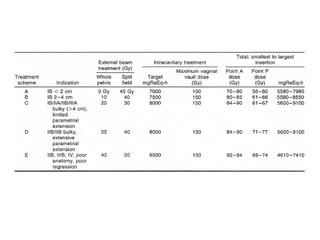
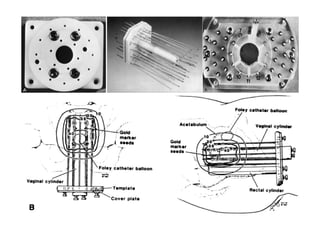
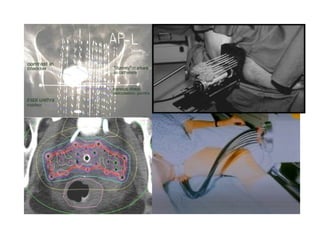
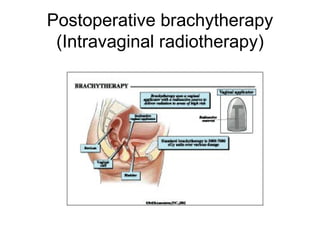
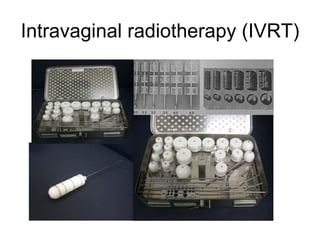
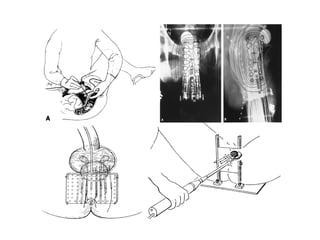
Brachytherapy involves placing radioactive sources close to or in contact with the target tissue and can be used to treat gynecological cancers. Common radioactive sources include radium-226, cesium-137, cobalt-60, iridium-192, and iodine-125. Brachytherapy is often used in combination with external beam radiation therapy and can be given as low dose rate brachytherapy over many hours or high dose rate brachytherapy over minutes. It allows high doses of radiation to be delivered to the tumor while sparing surrounding healthy tissues.