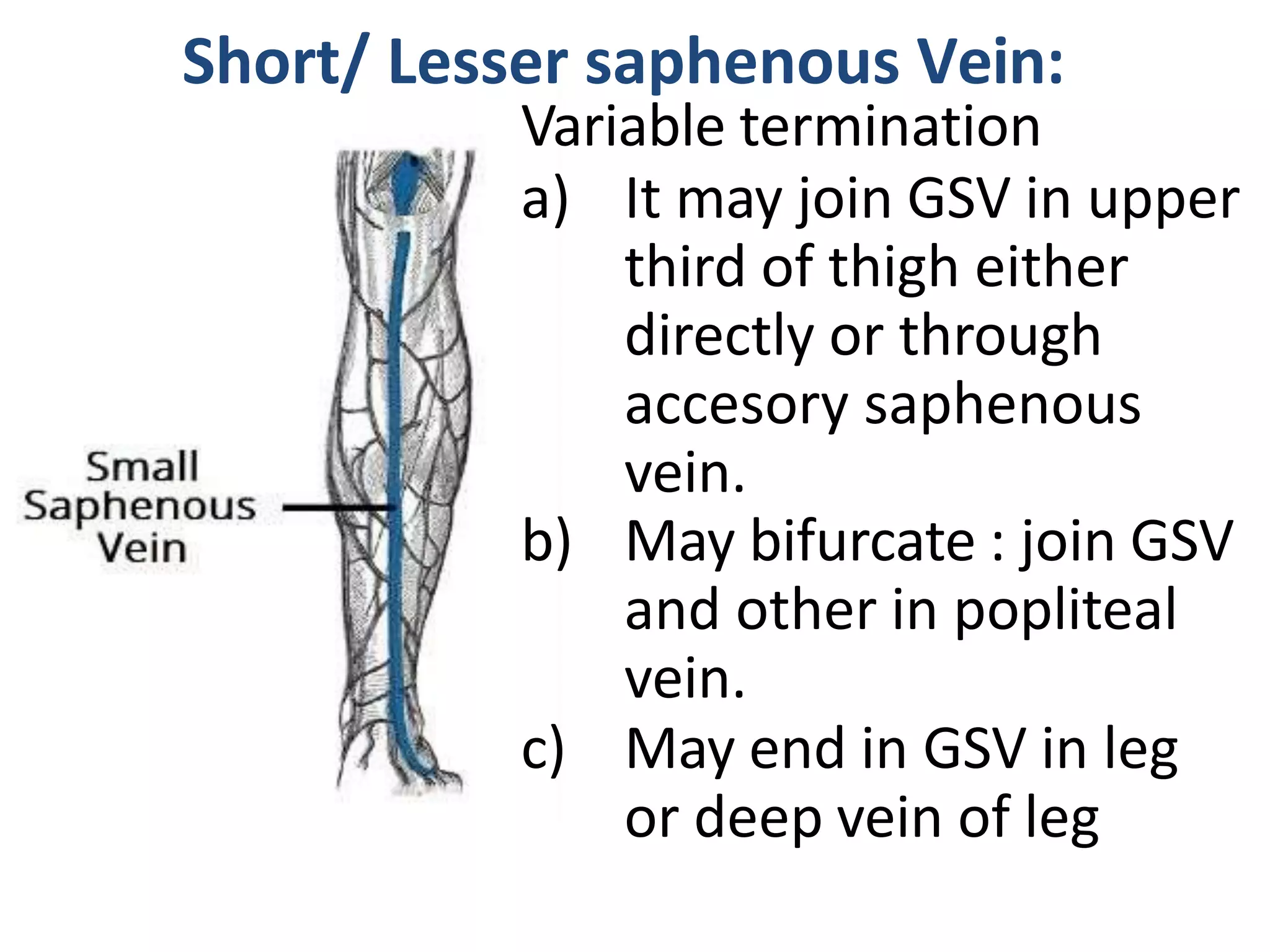
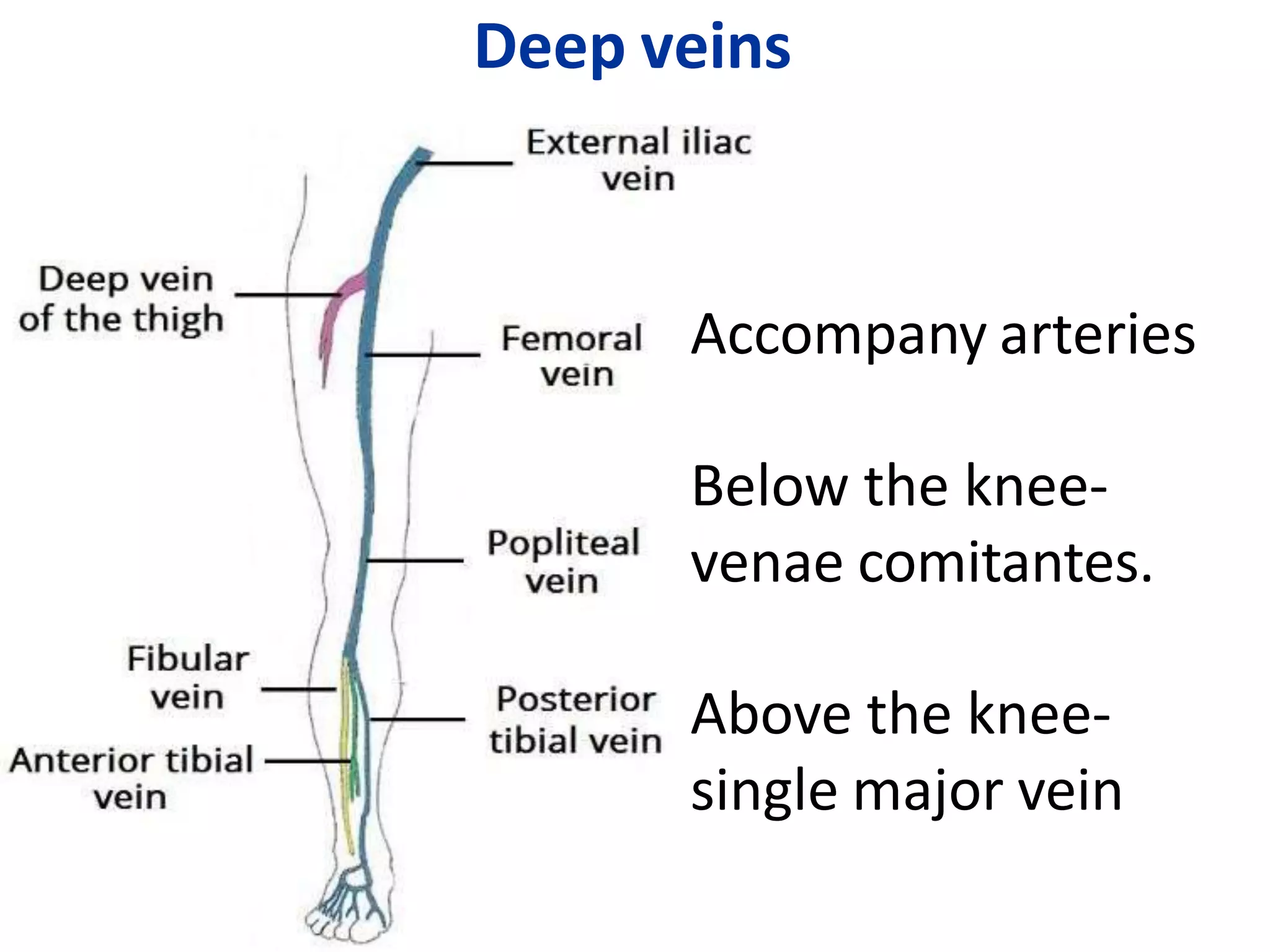
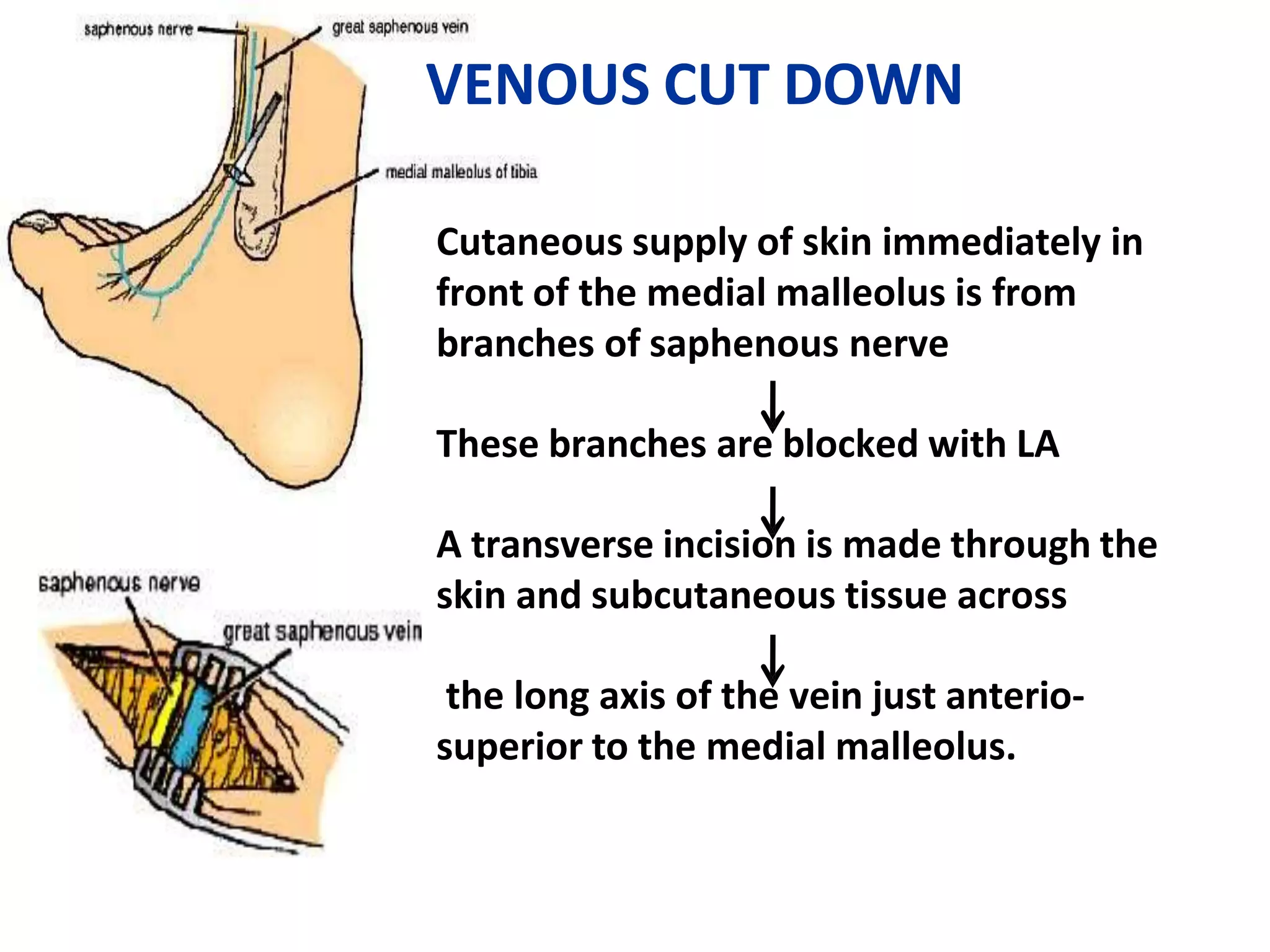
The document provides a comprehensive overview of the anatomy and blood supply of the lower limb, focusing on the femoral artery and its branches as well as the venous drainage system. It elaborates on various arteries and veins, including the great saphenous vein and the lesser saphenous vein, and discusses factors contributing to venous return and conditions like varicose veins. Additionally, it describes diagnostic tests for assessing venous incompetence, such as the Trendelenburg test and Perthes test.