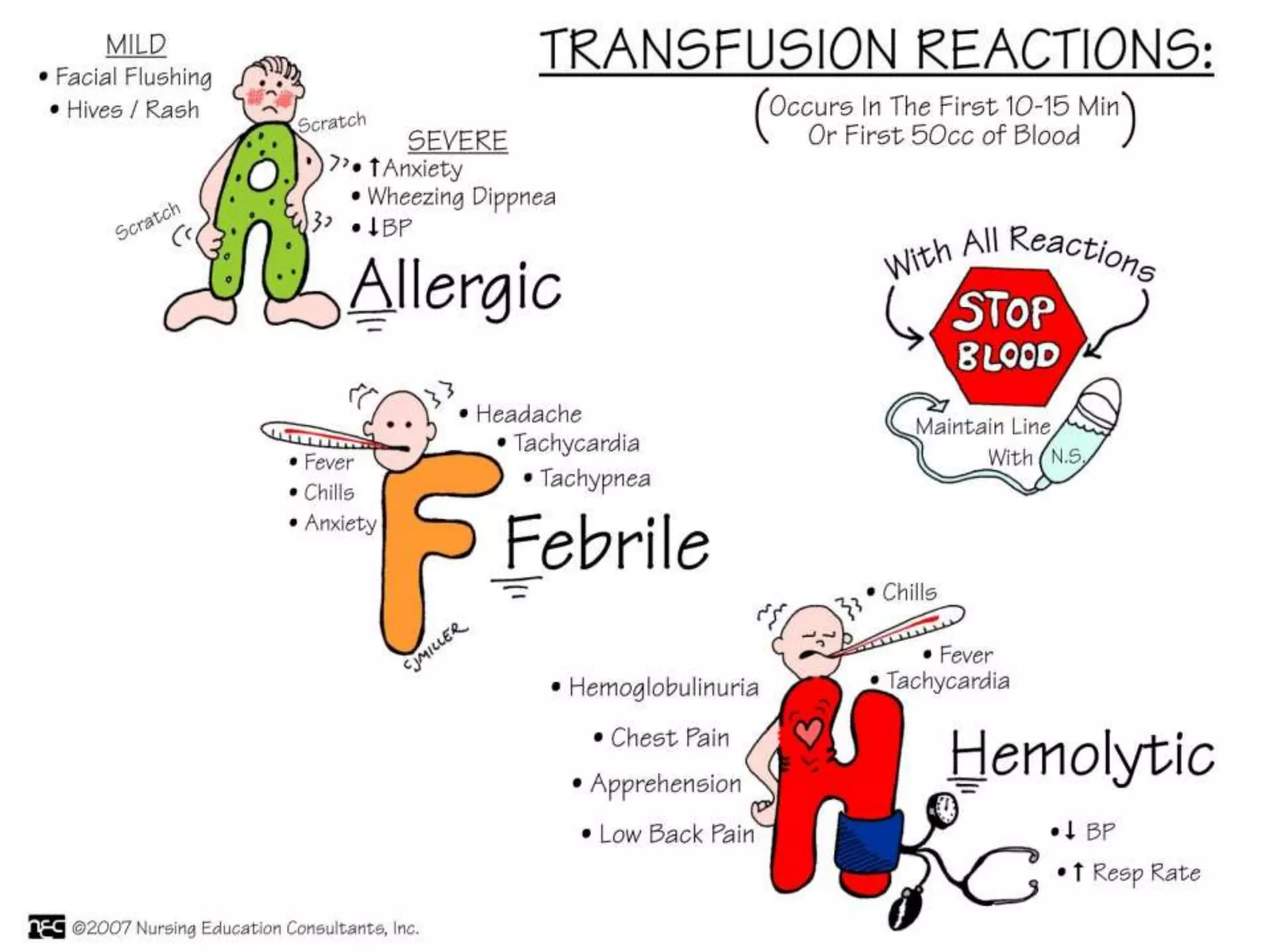
The document discusses the critical aspects of blood transfusion reactions, including types and management strategies for both immune-mediated and non-immune mediated reactions. It details specific conditions such as febrile non-hemolytic, acute hemolytic, delayed hemolytic, transfusion associated lung injury (TRALI), and graft-versus-host disease (GVHD), emphasizing their symptoms, diagnosis, and required emergency interventions. Recommendations for clinical management highlight the necessity of immediate action, monitoring, and supportive treatments in the case of transfusion complications.