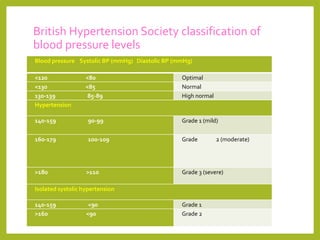
1) Blood pressure is measured in millimeters of mercury (mmHg) and recorded as the systolic pressure over the diastolic pressure. It is an important indicator of cardiovascular risk.
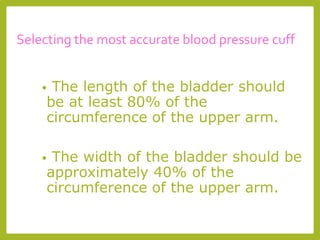
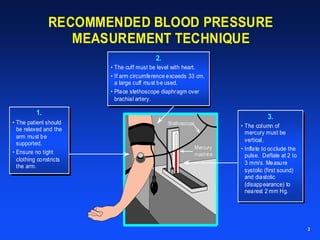
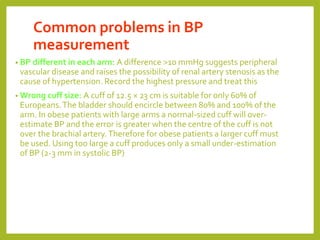
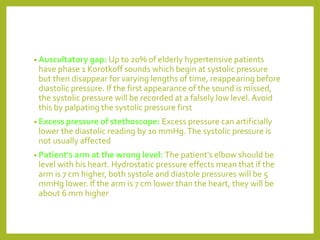
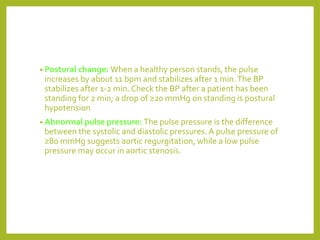
2) There are several factors that can affect the accuracy of blood pressure measurement, including using an incorrectly sized cuff, having the patient's arm at the wrong level, and excessive pressure from the stethoscope.
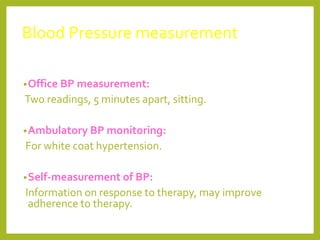
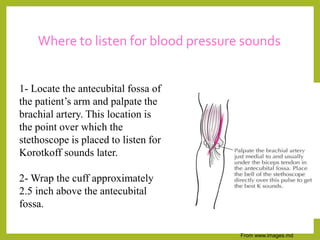
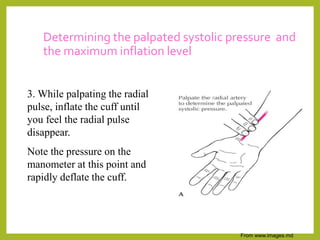
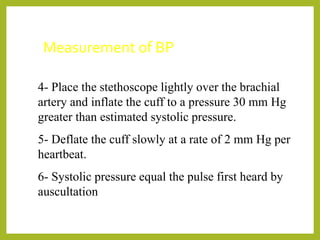
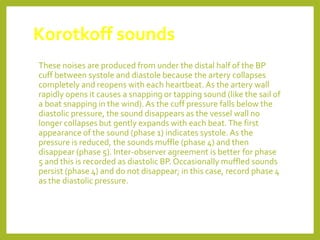
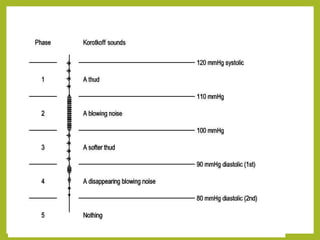
3) It is recommended that blood pressure be measured with the patient relaxed and supported, using the correct cuff size at heart level, and listening for Korotkoff sounds over the brachial artery to determine systolic and diastolic pressures.