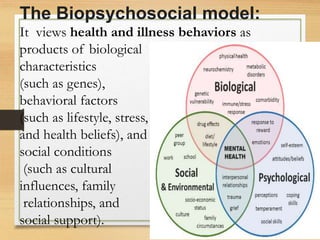
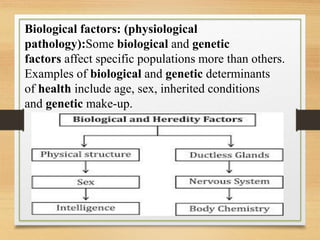
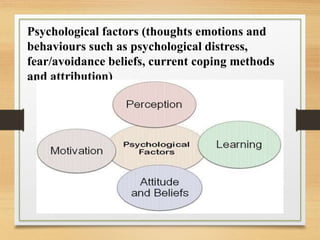
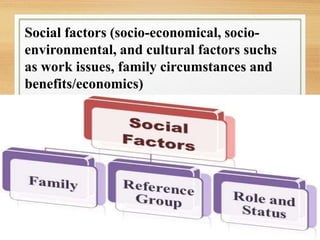
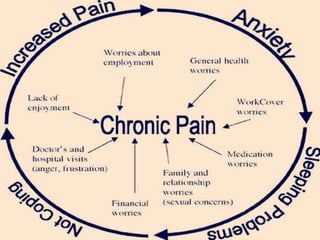
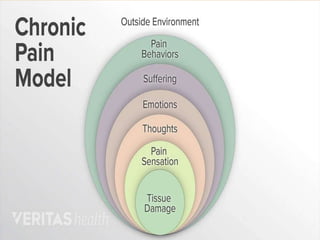
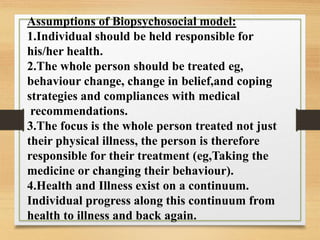
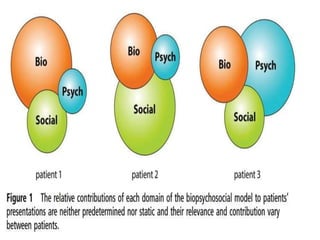
The document discusses models of health psychology, focusing on the biopsychosocial model. The biopsychosocial model views health and illness as influenced by biological, psychological, and social factors. It was first proposed by George Engel in 1977 as an alternative to purely biomedical models. The model examines the interconnections between biology, psychology, and socio-environmental factors in topics like health, disease, and human development. Strengths include improved patient outcomes, while limitations include being time-consuming and lacking a strong theoretical basis.