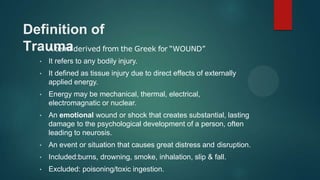
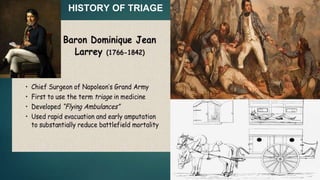
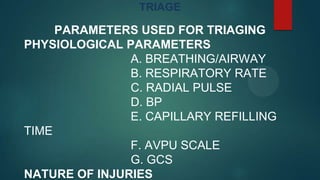
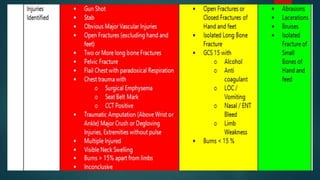
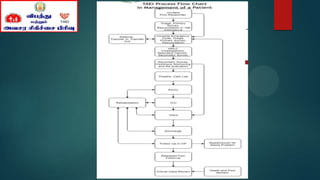
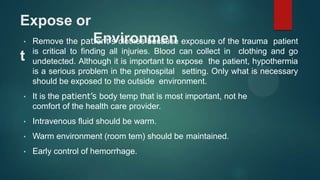
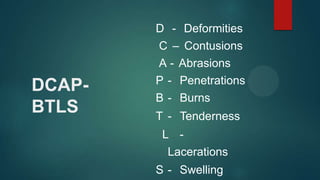
This document provides information on basic trauma life support. It defines trauma as any bodily injury, especially those caused by external forces. It discusses the history of triage, which involves sorting patients based on the severity of their injuries. Patients are categorized into red, yellow and green groups. Vital signs and the nature of injuries are used to determine the triage category. The primary and secondary surveys are described, which involve assessing the airway, breathing, circulation, disability and exposure. Specific injuries like bleeding, fractures and soft tissue injuries are discussed.