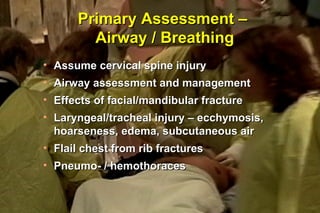
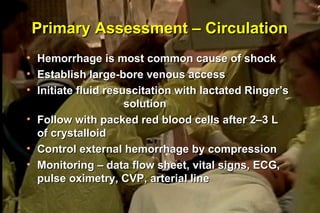
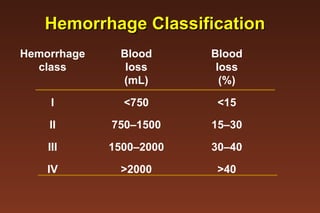
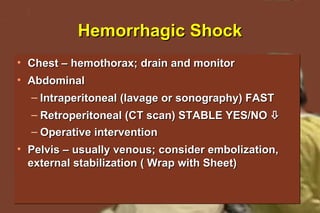
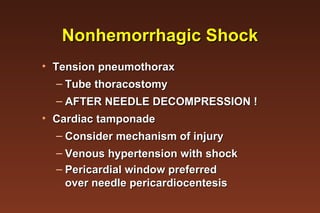
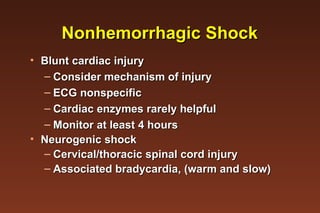
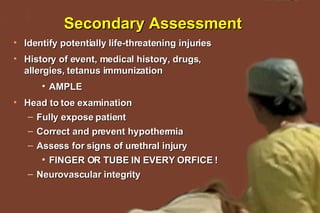
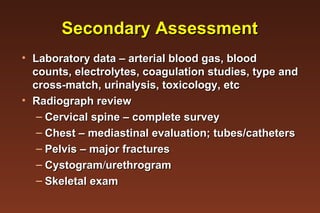
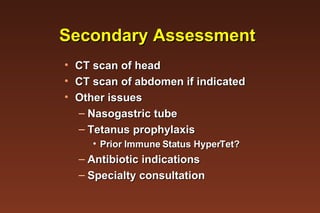
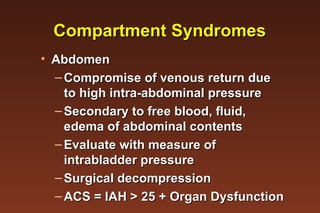
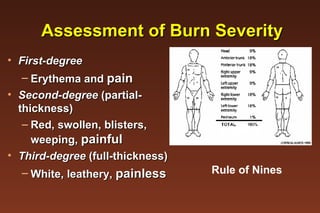
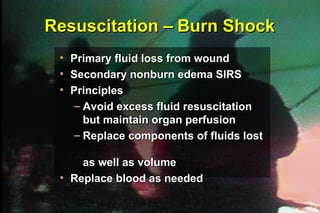
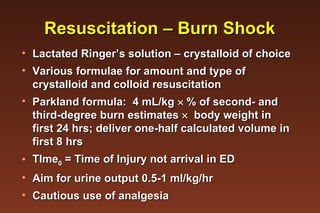
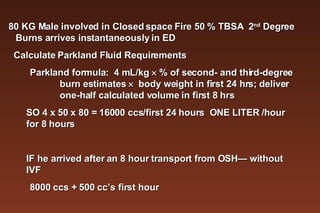
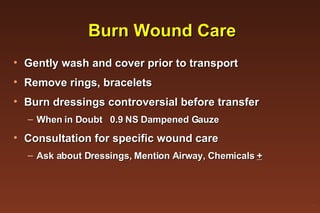
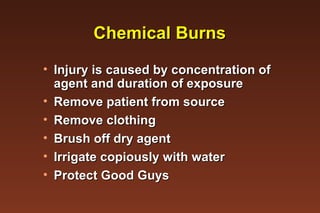
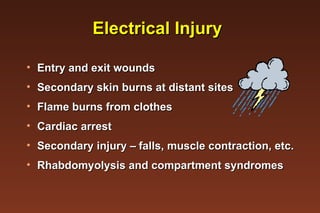
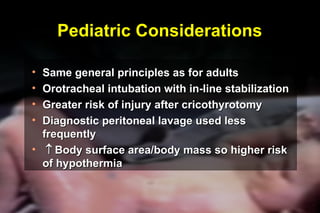
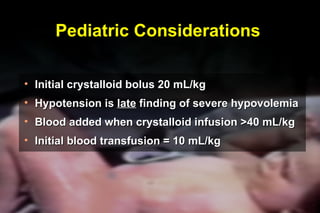
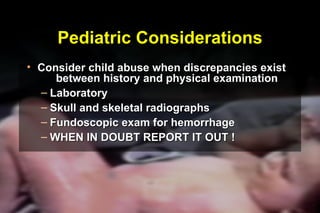
The document outlines the assessment and treatment of trauma and burn patients, including the primary and secondary surveys to address life-threatening injuries, guidelines for fluid resuscitation in burn shock, and key considerations for special populations like pediatrics. Standardized approaches are recommended to simultaneously assess airway, breathing, circulation, hemorrhage, and potential internal injuries while monitoring for changes in status. Early involvement of surgical specialists and use of radiography to identify fractures and hemorrhages are also discussed.