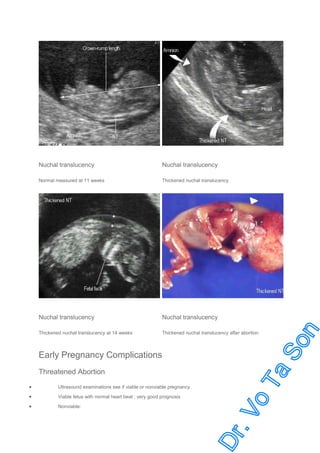
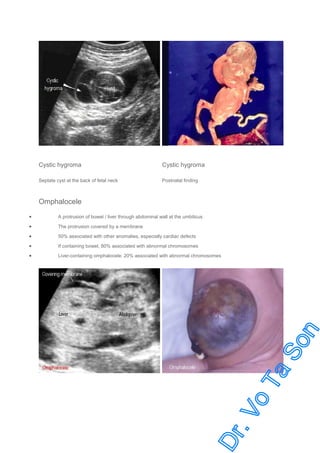
Ultrasound is a vital tool in obstetric practice for gestational age estimation, fetal growth monitoring, and anomaly screening, with routine screening performed at 18-20 weeks. Key indications include diagnosing pregnancy, assessing fetal development, and guiding invasive procedures, alongside evaluating complications like threatened abortion and ectopic pregnancy. The document outlines detailed fetal biometry parameters, ultrasound findings for various conditions, and the significance of amniotic fluid and placental assessments in managing pregnancy.