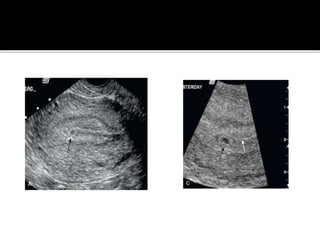
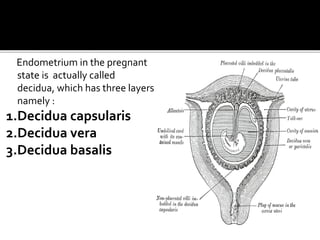
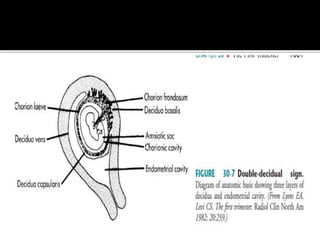
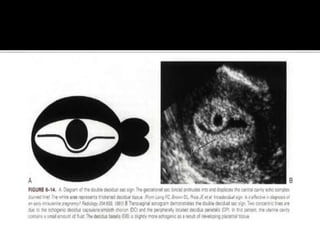
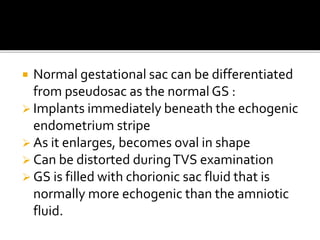
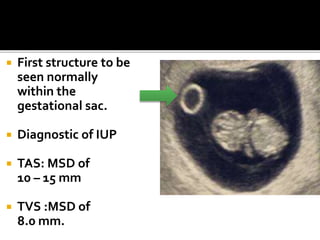
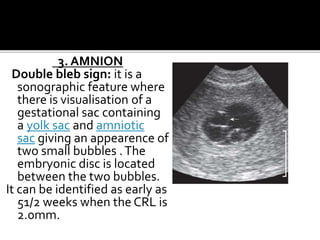
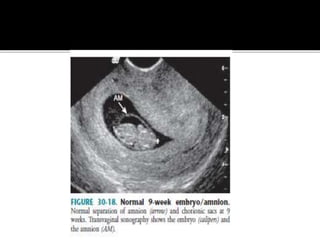
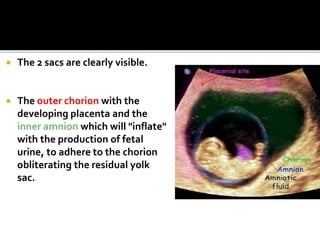
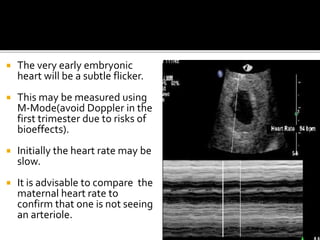
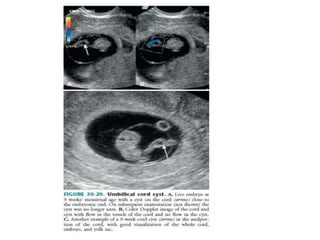
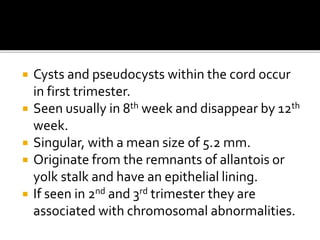
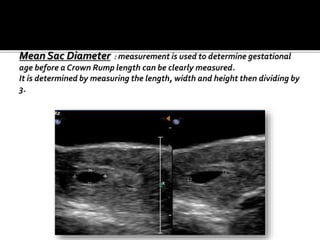
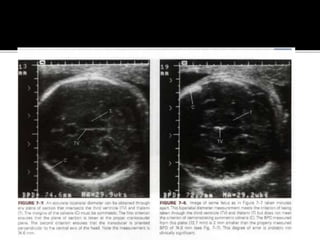
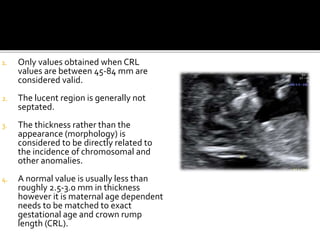
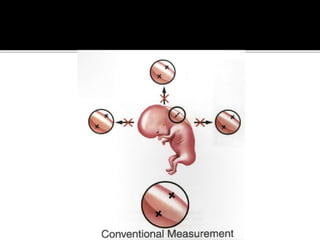
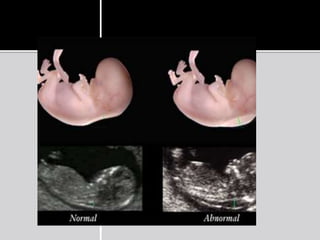
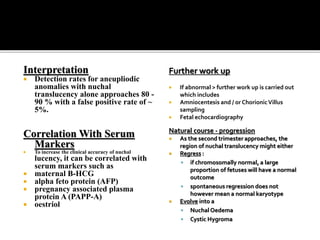
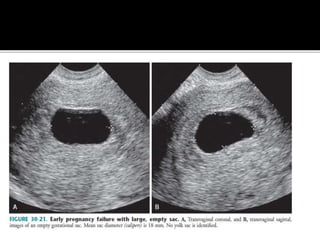
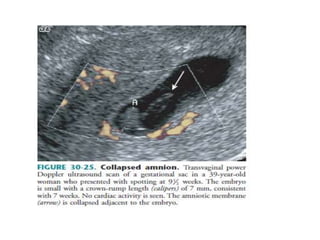
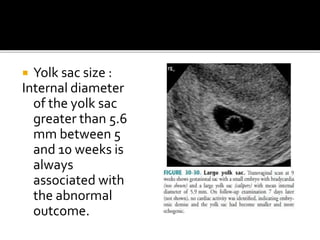
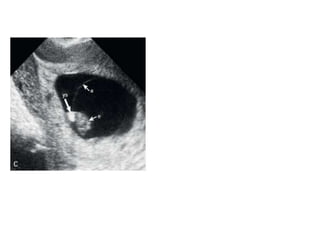
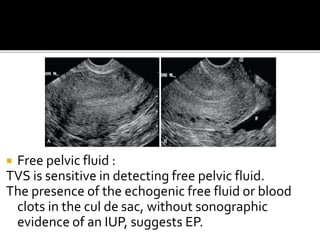
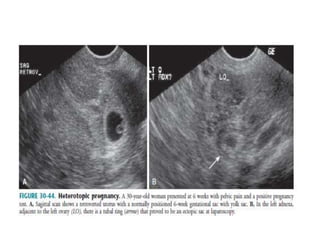
The document discusses ultrasound assessment of the first trimester of pregnancy. It defines the first trimester as the first 12 weeks and describes the typical sonographic appearance and development of the gestational sac, yolk sac, embryo, amniotic sac, cardiac activity, and umbilical cord. It outlines measurements used to date the pregnancy, including mean sac diameter, crown-rump length, and biparietal diameter. The document also discusses using nuchal translucency to screen for chromosomal abnormalities between 11-14 weeks.